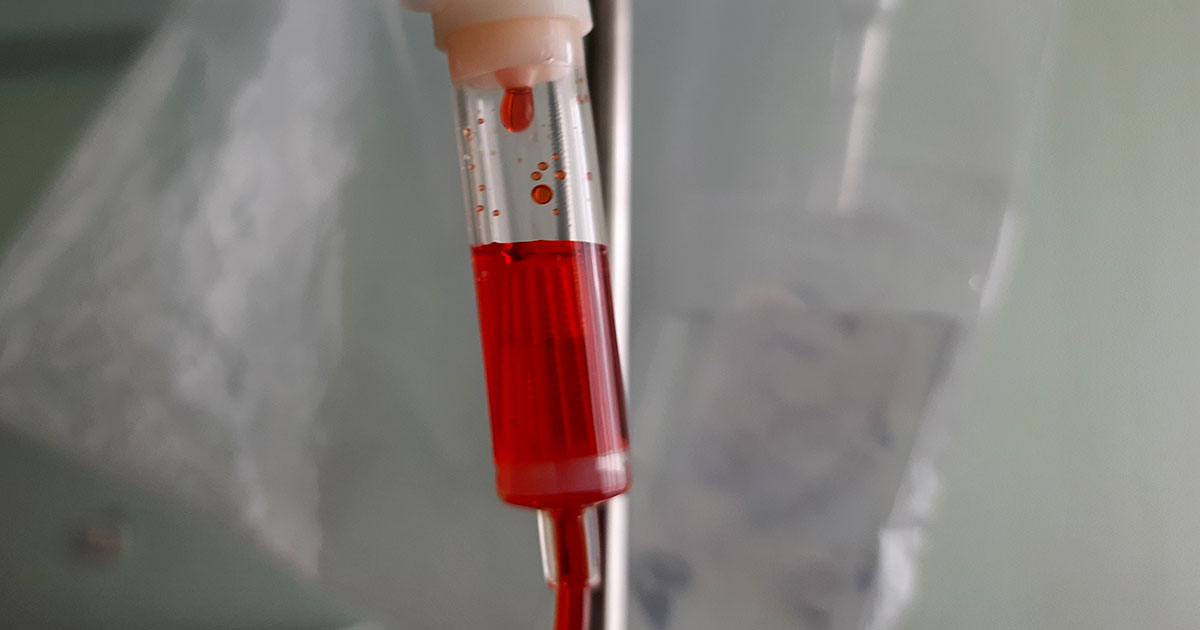
Chemotherapy is widely known to cause difficult side effects in most cancer patients, including hair loss, an increased risk of infection, nausea and vomiting. But one particular drug, doxorubicin, is so powerful and may produce such intense side effects it is named for Satan himself, and not just because of its bright red color.
The drug is commonly called the “red devil chemo” both because of its distinctive color and because it can cause serious side effects, including potential heart damage, in some individuals. Doctors carefully test patients before giving them doxorubicin to see if they are likely to be vulnerable to the heart effects.
In this article, we’ll explore:
- What is doxorubicin
- Is red devil the strongest chemotherapy?
- Doxorubicin side effects
- What to expect from red devil chemo
- Managing red devil chemotherapy side effects
If you’ve been diagnosed with cancer and want to get a second opinion about your diagnosis or treatment options, call us or chat online with a member of our team.
What is doxorubicin?
Doxorubicin is an antibiotic and potent chemotherapy drug that has been used to treat cancer since the 1960s. It’s part of a group of chemotherapy drugs called anthracyclines, medications which stop cancer cells’ growth by blocking an enzyme that’s necessary for cancer cells to divide and multiply. It is given as a liquid injected into the vein.
Doxorubicin is commonly used as an option to treat many types of cancer, especially once they have become metastatic, which means they have spread to other parts of the body. Among the common cancers it’s used to treat:
People with cancer often receive doxorubicin at the same time as other chemotherapy drugs. However, patients should not take some prescription drugs at the same time as doxorubicin and should tell their doctor about all medications and supplements they currently or have previously taken.
Is red devil the strongest chemotherapy?
Doxorubicin is one of the most powerful chemotherapy options for a wide range of cancers. Because of the way it works, doxorubicin can kill cancer cells at any point in their life cycle. It also stops cells from being able to reproduce. When a cell unwinds its strands of DNA to replicate, doxorubicin attaches itself to the DNA, putting itself between the DNA and the enzyme needed for replication.
A study in the Journal of Pharmacy and Pharmacology notes that doxorubicin is “regarded as one of the most potent of the Food and Drug Administration-approved chemotherapeutic drugs.” Its primary limitation, the article states, is its toxicity to non-cancerous cells in the body. Researchers have therefore been investigating ways to reduce its toxicity so that the drug can effectively attack cancer cells without posing as much risk to the heart.

Doxorubicin side effects
The most common side effects include nausea and vomiting, hair loss, low blood cell counts and mouth sores. The lower levels of platelets and red and white blood cells may lead to other side effects, such as looking pale and a risk of bleeding.
Other common side effects that occur in at least 10 percent of patients include:
- Breathlessness and a pale complexion, usually due to anemia, or a decrease in the body’s red blood cells
- Bruising, bleeding gums or nosebleeds, due to a decrease in the number of blood platelets, the part of blood that causes clotting and stops bleeding
- Fatigue and weakness
- Loss of appetite
- Diarrhea or constipation
- Fever
- Redness, soreness or peeling on the hands and soles of the feet
- Changes in heart rate
- Mild, temporary changes to the liver
- Weight gain
Other side effects are less common. Fewer than 10 percent of patients experience changes to their nails, inflammation around the injection site, sore eyes, stomach/abdominal pain, feeling thirsty, dizziness, burning or tingling in the hands or feet, or heart damage, including heart failure. Doxorubicin can also cause changes to the menstrual cycle and temporarily stop sperm production.
A possible complication when receiving doxorubicin is leakage out of the vein into the surrounding tissue, sometimes causing blisters or sores. This is called extravasation and is treated with elevating the site and putting a dry, cold compress on the site for 20 minutes. Medications for this complication include dexrazoxane hydrochloride or topic dimethyl sulfoxide. If blisters, ulcers or ongoing pain occur, it may be necessary to remove the damaged tissue.
About one in 10 people develop heart problems from doxorubicin within a few days of receiving it. About one in four people will experience an irregular or rapid heartbeat or swelling in the heart which will go away. In rare cases, people can develop heart problems a few months or up to 20 years after getting doxorubicin.
The most severe type of heart problems that can be caused by doxorubicin, such as congestive heart failure, occur in about one out of 50 to 100 people. The risk of congestive heart failure is higher with high doses of the drug, in very young or very old patients, when the drug is combined with others that can cause heart problems, or in those who already have heart problems or high blood pressure.
Very rare side effects, occurring in less than one out of 100 people, include inflammation of a leg vein, blood clots, fluid around the heart or developing of a type of blood cancer called acute myeloid leukemia. In rare cases, receiving doxorubicin can cause tumor lysis syndrome, which means the tumor cells release their contents into the blood.
Patients who experience the following symptoms should see a clinician immediately:
- A rapid or irregular heartbeat
- Bloody or black stools
- Hives
- Itching
- Seizures
- Shortness of breath
- Skin rash
- Sore throat
- Swelling in the hands, feet, ankles or lower legs
- Trouble breathing or swallowing
- Ongoing cough, congestion or other symptoms of an infection
- Unexpected bruising or bleeding
- Vomit with blood in it or with dark brown material that looks like coffee grounds
What to expect from red devil chemo
Doxorubicin is usually given in 21-day cycles, but some people may get it every 28 days. The number of cycles patients receive of doxorubicin depends on their type of cancer, other drugs they are receiving and their treatment plan. For example, most people with breast cancer will receive four cycles.
Before receiving doxorubicin, doctors conduct tests to determine the patient’s blood cell levels and kidney and liver function. Patients also undergo an electrocardiogram, which records the heart’s electrical activity, and an echocardiogram, an ultrasound imaging test to see how well the heart pumps blood.
About an hour before an appointment, taking an anti-nausea medication or wearing an anti-nausea skin patch may help patients reduce the likelihood of nausea or vomiting. Patients should ask their doctor about the drugs they recommend to reduce nausea.
Doxorubicin is given to patients through one of three methods.
One method uses a long plastic tube that enters a large vein in the chest, either a central line, a PICC line, or a portacath.
A second method uses a cannula, a thin short tube, that enters a vein in the arm.
A third method, mainly used for bladder cancer, uses a catheter to administer the drug directly into the bladder.
When patients arrive to receive their treatment, a healthcare provider will take their vital signs and help them find a comfortable position. Then they will insert the tube used to give the medication. It usually takes about 15-20 minutes to inject a dose of doxorubicin, but it can take longer.
For the next few days after treatment, a patient’s urine might be pink, reddish, orange or brownish. This is normal and will go away after a couple days.
People who have received doxorubicin cannot receive live vaccines, such as the measles or shingles vaccines, for up to one year after treatment. They can receive flu vaccines, COVID-19 vaccines and other non-live vaccines.
Managing red devil chemotherapy side effects
Side effects vary for every individual. Patients should talk to their medical team about any side effects they experience so that they can help manage them. Keeping track of symptoms in a notebook or diary can help patients remember what to tell them and know what to expect during the next treatment cycle.
Certain lifestyle behaviors can help with all kinds of side effects:
- Get some physical activity each day, such as a short walk.
- Avoid over-exertion with intense exercise.
- Try to maintain a regular sleep routine with the same bedtime and wake time each day.
- Take short naps to combat fatigue or sleepiness, but try to keep them to about 30 minutes.
- Rest when feeling fatigued or the need for a break.
- Avoid alcohol and caffeine.
- Stay hydrated with lots of water or other fluids.
- Regularly wash hands to reduce the risk of infections.
- Wear a protective face mask, such as an N95 or KN95, in public indoor spaces during flu season and during spikes in Covid-19, to reduce the risk of catching these and other respiratory diseases.
- Seek out a support network and ask others for help with household routines and chores.
- Spend enough time with people to avoid loneliness, but patients shouldn’t be afraid to tell someone when they need to be alone.
Nausea may be treated with anti-nausea medications, including skin patches that can be worn for several days. But, patients should make sure the ones they take will not interfere with treatment. Ask the medical team what anti-nausea drugs they recommend for the particular treatment plan. Taking these drugs regularly, even when patients don’t feel sick, may reduce the chances of developing nausea.
Other ways to reduce the likelihood of nausea include:
- Avoid eating just before your chemotherapy treatment. Have a small meal or large snack a few hours afterward instead.
- Avoid fried foods, fatty food, or foods with a strong smell.
- Avoid being around food when feeling sick.
- Eat smaller meals and snacks throughout the day instead of large meals.
- Drink carbonated drinks, especially ones with ginger.
- Suck on hard candies.
- Eat a banana to replace potassium levels after vomiting.
Sometimes anti-anxiety medications, such as benzodiazepines, can help with nausea as well. If the anti-nausea drugs don’t work, a doctor might prescribe nabilone, a cannabis-based medication.
The following might also help relieve nausea:
- Acupuncture or acupressure
- Cognitive behavioral therapy
- Reading or listening to books, playing video games, watching TV or listening to music can all be helpful distractions
- Yoga
- Muscle relaxation training
- Exercise
- Hypnosis
To prevent mouth sores, get a dental cleaning and check-up before treatment begins and follow these tips:
- Check your mouth daily for sores or white spots, and let your medical team know about any sensitive areas or pain.
- Use a soft toothbrush to brush your teeth, gums, and tongue twice daily.
- Patients who experience bleeding with a soft toothbrush should use cotton swabs instead.
- Sucking on ice chips during treatment may reduce the risk of mouth sores, according to a 2019 study.
- Avoid alcohol-based mouthwashes. Instead, try rinsing the mouth every three hours with a mixture of warm water (1 cup), baking soda (1/4 teaspoon) and salt (1/8 teaspoon). Patients who have bleeding or are at risk of bleeding should ask their medical team if they should floss.
Hair loss is very common with doxorubicin. People have different ways of adjusting to losing their hair. Cutting hair short before treatment begins might help patients get used to having less hair. Some people even shave their heads before treatment starts. Some prefer to wear scarves or a bandana, and others prefer to use a wig. Some hospitals offer cooling caps, which may reduce hair loss by constricting follicle cells, making them more difficult for the drug to penetrate.
Follow these tips to manage hair loss:
- Once treatment starts, wear a hair net while sleeping so that hair falling out is captured in the net instead of getting on the pillow.
- For a dry or itchy scalp, rub moisturizer or oil in it.
- Avoid using hair dyes, hair chemicals, and heated styling devices, such as curling irons.
- Use gentle shampoos, such as a baby shampoo.
- Use sunscreen when the scalp is exposed to the sun.
- Wear a warm hat when temperatures drop. In cooler weather, consider wearing a cap to bed to keep warm.
If you’ve been diagnosed with cancer and want to get a second opinion about your diagnosis or treatment options, call us or chat online with a member of our team.



