Any good carpenter will tell you to use the right tool for the right job. An oncologist will tell you the same thing. Doctors who treat cancer have a variety of drugs, devices and other options in their toolbox depending on the patient and the type and stage of cancer. Using the correct cancer-fighting tool or tools is critical for oncologists to help position their patients for the best outcomes possible.
Among the most common tools doctors employ are chemotherapy and immunotherapy—two cancer-fighting treatments that use very different approaches. How do they differ?
- Chemotherapy kills fast-growing cells—both cancerous and non-cancerous—in the body.
- Immunotherapy helps the immune system do a better job of identifying cancer cells so it can attack and kill them.
“Chemotherapy is a reactive approach. There’s a fast-growing cancer cell in your body, so you want to stop the fast-growing cells. You use chemo to get rid of them, hoping that you will get all the cancer cells at the same time,” says Arturo Loaiza-Bonilla, MD, Vice Chairman of the Department of Medical Oncology at Cancer Treatment Centers of America® (CTCA). “Immunotherapy, in theory, uses your own body, which is very well-trained through evolution. We are able to fight any kind of infection if we know how to identify the pathogen we’re attacking. Ideally, if you’re able to train your immune system to identify cancer, that’s the ultimate goal, because you’re using your own body to do the attacking.”
Both chemotherapy and immunotherapy may be used alone or together, or they may also be used in combination with other treatments, such as surgery or radiation therapy.
Chemotherapy drugs work while they’re being administered and remain in the body, while immunotherapy drugs may stimulate the immune system to continue attacking the cancer even after treatment has ended. Chemotherapy has a more immediate impact, shrinking tumors and killing cancer cells, while immunotherapy’s effects take place over a longer period of time.
“I don’t think necessarily that one’s better than the other; it’s just that we need to be smart about when we use one vs. the other or in combination,” Dr. Loaiza-Bonilla says.
In this article, we’ll explore:
- What is immunotherapy?
- Biomarkers that affect treatment decisions
- What is chemotherapy?
- What is targeted therapy?
- What are the side effects of these treatments?
- The comprehensive treatment approach at CTCA
If you have questions about immunotherapy, chemotherapy or other cancer treatments we offer, or if you’re interested in a second opinion on your cancer diagnosis and treatment regimen, call us or chat online with a member of our team.
What is immunotherapy?
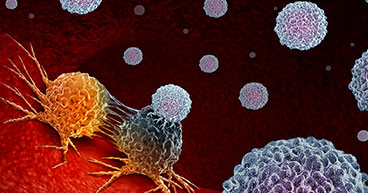
Cancer cells aren’t like typical cells in the body. They don’t die normally. They divide rapidly, over and over again, while frequently mutating and evading the immune system, which is supposed to protect you from disease and infections.
Immunotherapy drugs are designed to reveal these abnormal cells to the immune system, so it can get to work destroying them. Immunotherapy drugs cover a number of general categories:
- Checkpoint inhibitors: Cancer cells may send out signals that trick the immune system into thinking they’re healthy cells. Checkpoint inhibitors are designed to disrupt that signal, triggering an immune system response to the cancer.
- Cytokines: These protein molecules help regulate and direct the immune system. To beef up an immune response to cancer, cytokines are synthesized in a laboratory and then injected into the body in much larger doses than the body produces naturally.
- Cancer vaccines: These drugs reduce the risk of cancer by attacking viruses that cause cancer. They may also stimulate the immune system into attacking cancer cells in a specific part of the body.
- CAR T-cells (chimeric antigen receptor T-cells): These cells are infection-fighting T-cells that have been extracted from blood, re-engineered to attack cancer cells and then returned to the body. These modified T-cells, called CAR T-cells, are designed to attack specific features on cancer cells.
“If we can train our own bodies to identify the cancer and fight it as such, then we have the ultimate solution against the cancer because the immune system is always vigilant.” Dr. Loaiza-Bonilla says.
The science of immunotherapy is still evolving, and the treatment effectiveness is only available to some patients with specific cancers.
“Not everyone benefits from immunotherapy,” Dr. Loaiza-Bonilla says. “As a single agent, immunotherapy, particularly for solid tumors, is not as effective unless there’s a specific biomarker or something that tells us the immune system is being suppressed. Then, by using these agents, we can awaken the immune system so it can produce the effect we’re anticipating.”
Biomarkers that affect treatment decisions
Oncologists use biomarkers to help determine whether immunotherapy, chemotherapy or a combination of the two may be an appropriate treatment for a cancer patient. While researchers continue to look for other useful biomarkers, three of particular importance help determine whether immunotherapy is a treatment option. They are:
PD-L1: The biomarker PD-L1 is a protein that’s expressed in tumor cells, telling the immune system not to attack a particular cancer cell. If the PD-L1 expression level is high, say above 50 percent, then immunotherapy by itself may be recommended. The lower the percentage, the more likely the patient will undergo chemotherapy. However, even in those cases, immunotherapy may still be of some benefit. “When the numbers are low, chemotherapy can be used—that’s fine. But we can add immunotherapy to really enhance the response,” Dr. Loaiza-Bonilla says.
Microsatellite instability-high (MSI-H) or mismatch repair deficiency (d-MMR): All cells in our bodies have ways to repair damaged DNA using certain proteins, but some cancers develop because of a deficiency in those repair systems. Because the necessary proteins are not available to repair the DNA, lots of mistakes occur in the DNA. The more mistakes there are, the more likely the body is to create abnormal proteins that the immune system, when awakened, will recognize as abnormal. “With patients with these MSI-High features, we can use a combination of immunotherapies only. We don’t even need chemo,” Dr. Loaiza-Bonilla says. “They are better than chemo in fighting the cancer. For a number of patients, it sometimes leads to a sustained period where the cancer is no longer detected.”
Tumor mutational burden (TMB). With PD-L1, doctors conduct tests to determine the percentage of cells with that biomarker. With MSI-high, they check for the presence of four proteins that facilitate DNA repair. Tests for tumor mutational burden require a full genome readout, called next-generation sequencing. These tests measure the density of mutations in a tumor. The higher the concentration of mutations, the more likely immunotherapy will have an impact.
Dr. Loaiza-Bonilla compares the mutations in a tumor to typos on the pages of a book.
“Imagine the DNA is the body’s manual, written as a book. Instead of going to one page only to check on a gene, you actually read the whole book. You are going onto each page to see where the typos are. Those typos in a genome are mutations,” he says. “The more typos per page, or ‘mutations per megabase’ in that book, or that readout of the DNA by these techniques, the higher the chances you may respond to immunotherapy. When you awaken the immune system to check out the book, it sees all the typos and says, ‘We have to get rid of this.’”
What is chemotherapy?
Chemotherapy drugs are either systemic, traveling through the bloodstream to reach cancer cells, or they’re regional, meaning they’re directed to a specific area of the body.
Different chemotherapy drugs have different ways of stopping cancer cells from growing and replicating. “Chemotherapy as a whole is aimed at disrupting the cell replication process during different parts of the cell cycle, when it’s trying to split in two or divide,” Dr. Loaiza-Bonilla says.
Chemotherapy may be used as the primary treatment to destroy cancer cells in the body or to relieve symptoms of advanced cancer. It may be used before other treatments, such as surgery or radiation therapy, to shrink a tumor. It may also be used after other treatments to destroy cancer cells that remain. Chemotherapy may be needed when cancer cells have returned or spread to other parts of the body.
“Chemotherapy still has a significant role to play and is very effective, particularly to prevent cancers from coming back,” Dr. Loaiza-Bonilla says. “Chemotherapy is here to stay; we’re just modulating it and changing the dosing and the schedule, but there will always be some form of chemo that we use on a number of patients.”
What is targeted therapy?
Immunotherapy is a type of precision medicine. Another precision medicine treatment for cancer is targeted therapy. The drugs used in targeted therapy seek out features unique to specific cancer cells—or cells that influence the behavior of the cancer cells. These therapies are specific either to the particular cancers they affect or to specific features of cancer cells no matter where they appear in the body.
Your doctors will perform advanced genomic testing and other laboratory tests and diagnostic procedures to determine whether there’s an available targeted therapy that may benefit you.
Monoclonal antibodies are used in some forms of targeted therapy. These laboratory-engineered molecules attach to specific targets, also called receptors or proteins, found on cancer cells. Some may stop the cancer cells from growing, while others may lead the cancer cells to self-destruct. Sometimes, these monoclonal antibodies are used to carry chemotherapy or radiation drugs directly to the tumor cells to kill the cancerous cells.
Targeted therapy may also be used to prevent cancer cells from making new blood vessels, cutting the cells off from the nourishment they need. Other targeted therapies may stop the production of hormones that help tumors grow.
What are the side effects of these treatments?
Any form of cancer treatment may have side effects. Because chemotherapy doesn’t target just cancer cells, but all cells that divide rapidly, it may also damage fast-replicating hair, skin, blood and intestinal cells. That’s why hair loss, anemia and nausea are common side effects of chemotherapy treatments.
With immunotherapy, some side effects are caused by the drugs putting your immune system into overdrive, sometimes to the extent that your immune system attacks your organs.
“Cancer is serious business. We’re on top of our patients all the time. We need to educate them on how certain side effects may be more prominent than others, depending on the modality of treatment we’re using,” Dr. Loaiza-Bonilla says.
Chemotherapy and immunotherapy often cause many similar side effects, including:
Other symptoms—some flu-like—are also possible following immunotherapy. These include:
- High blood pressure
- Fluid buildup (lymphedema), usually in the legs
- Fever or chills
- Pain or weakness
- Headaches
- Rashes or itching
- Fatigue
- Nausea or vomiting
- Diarrhea
- Mouth sores
Other chemotherapy-related side effects may include:
- Weight loss or weight gain
- Hair loss
- Anemia
- Weakened immune system, which may lead to infections
The side effects of immunotherapy generally become less severe after the first treatment. For chemotherapy, most side effects subside once treatment is completed.
“One advantage of chemo is that the side effects appear when the treatment starts, but once you stop the chemo, most of those side effects go away. They’re dose-dependent, they’re timing-dependent,” Dr. Loaiza-Bonilla says. “When you’re using immunotherapy, you may have no side effects, which would be great, but on the other hand, you may have those random idiosyncratic reactions that are autoimmune phenomena that happen to the patient because the immune system was awakened. The good thing is we know how to handle those side effects, too. We’re basically toning down the system in those cases.”
The comprehensive treatment approach at CTCA
Patients who come to CTCA for cancer treatment are given whole-person care, meaning their care team not only determines appropriate therapies to treat the disease, they also offer evidence-informed supportive care services designed to patients help manage their symptoms and side effects and maintain their quality of life.
Using laboratory tests, advanced genomic testing and other means, our multidisciplinary team of cancer experts thoroughly evaluate patients to determine which treatment is right for them based on biomarkers, mutations or other genetic features found in their cancer.
“We need to do testing for patients to determine whether we would recommend immunotherapy or chemotherapy, or a combination those or other treatments,” Dr. Loaiza-Bonilla says. “We need to do comprehensive genomic panels. We need to check for the protein expression of certain biomarkers, because that’s the personalized approach that patients deserve.”
Similarly, each patient’s treatment regimen includes recommended supportive care services designed to meet their specific needs—whether they’re undergoing immunotherapy, chemotherapy, other treatment or a combination of multiple treatment options.
For instance, a pain management physician may help immunotherapy patients reduce or prevent headaches and other discomfort. Chemotherapy patients, meanwhile, typically work with an oncology-trained nutritional support provider who helps them develop an eating plan designed to ensure they get the nutrients they need, especially if they experience nausea and loss of appetite.
“Our dietitians provide diet counseling intended to help individuals choose more nutritious plant-based foods,” says Carolyn Lammersfeld, Vice President of Integrative Care at CTCA. “Also, some supplements should not be taken while a patient is on immunotherapy. Our team of registered dietitians and naturopathic providers provide advice on what is safe to take during treatment.”
If you have questions about immunotherapy, chemotherapy or other cancer treatments we offer, or if you’re interested in a second opinion on your cancer diagnosis and treatment regimen, call us or chat online with a member of our team.