Cancer cells are, by their nature, defective. They are once-healthy cells that are broken and no longer have working safeguards that prevent them from repairing themselves or growing out of control. To survive inside the body, and evade our immune system defenses, these defective cells often rely on nearby healthy tissue for survival and protection and to thrive, grow and spread.
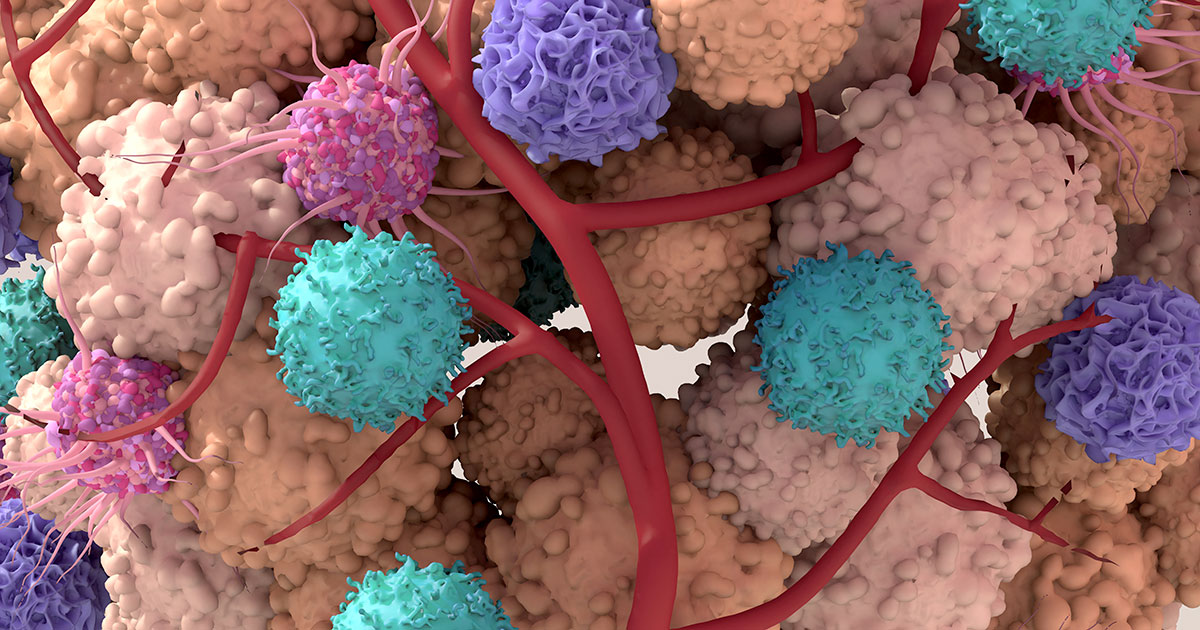
This ecosystem surrounding cancer cells is called the tumor microenvironment (TME)— a complex, biological metropolis of cells, molecules, proteins and blood vessels. While portions of the TME work to eliminate the cancerous cells, they are often outmaneuvered by other parts of the TME that help get nutrients to the cancer cells or suppress any immune system attacks.
Researchers have increasingly focused on the TME’s role in cancer development in their quest to find new treatments. In addition to administering drugs that can kill cancer cells, successful therapies must also overcome obstacles in the TME that aid a tumor, so that the cancer-fighting drugs can reach their target.
For instance, a recent study from the Institute for Research in Biomedicine in Spain found that colorectal cancer patients develop resistance to platinum-based chemotherapy because much of the drug may accumulate in healthy cells in the TME and never reach its intended target.
“This study is an important step toward understanding why chemotherapy does not work the same way in all cancer patients,” Dr. Clara Montagut, head of the gastrointestinal tumor section at Hospital del Mar in Barcelona, writes in the study report. “This work is also essential in demonstrating that cancer treatment must take into account not only the cancer cells but also the healthy cells in the tumor.”
That’s often why doctors may turn to treatment combinations that target cancer cells and supporting TME components (called the stroma).
In this article we will cover:
- What is a tumor microenvironment?
- Tumor microenvironment and cancer types
- The future of TME research and therapueutics
If you’ve been diagnosed with cancer and are interested in a second opinion about your diagnosis or treatment plan, call us or chat online with a member of our team.
What is a tumor microenvironment?
The National Cancer Institute describes the tumor microenvironment as “the normal cells, molecules and blood vessels that surround and feed a tumor cell.” Not only can a tumor change its microenvironment, but “the microenvironment can affect how a tumor grows and spreads,” the NCI says.
Think of cancer cells as a crime syndicate that pops up in a neighborhood and gains a foothold while keeping a low profile. The syndicate may tap into the wider community by paying off law enforcement, extorting store owners for their “protection” and posing as “legitimate businessmen.” Emboldened by its success, the syndicate eventually looks for ways to grow and expand its territory.
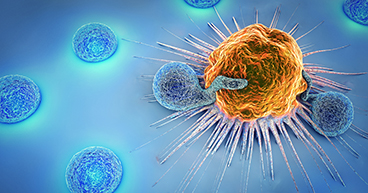
Consider the TME as a cancer’s neighborhood. Once cancer cells are established in a part of the body, they begin to take advantage of healthy cells around them. That may mean co-opting regulatory T-cells (T-regs) that are designed to suppress the immune system and reduce the chances of an attack. It may mean promoting tumor-associated macrophages (TAMs) that secrete vascular endothelial growth factor (VEGF), which helps form new blood vessels (angiogenesis) to carry more nutrients to the cancerous cells.
You may think that having lots of immune cells in the microenvironment would make it difficult for cancerous cells to survive, but many of the disease-fighting immune cells that we rely on to suppress tumor growth can also promote it under the right conditions. The TME has many ways of suppressing the immune system, as reported in the April 2020 edition of Current Biology, reducing the effectiveness of many cancer therapies.
Tumor microenvironment and cancer types
Knowing the composition of a TME for a specific cancer may help “predict a patient’s clinical outcome,” says a 2018 report in the British Journal of Cancer. For instance, studies have shown that multiple myeloma disease progression is greatly affected by the tumor microenvironment. In chronic lymphocytic leukemia, the structure of the TME promotes the disease and compromises any immune response to the cancer. And with B cell lymphomas, using biomarkers to develop immunotherapy strategies such as checkpoint inhibitors have partly resulted from a better understanding of the tumor microenvironment.

The future of TME research and therapeutics
NCI researchers have found that therapy approaches targeting some problem cells in the TME may also have a negative systemic impact on the same type of cells outside the TME. Because of this, they say the goal of therapy should be to “‘manage’ the TME for maximum benefit and minimum risk.”
An October 2022 NCI report noted: “There are new treatment options including small molecular weight drugs, antibody-based agents and transduced lymphocytes, each employed with the goal of improving outcomes for patients with cancer.”
The report suggested five potential strategies for achieving TME management, depending on the type of tumor. They are:
- Turn a so-called “cold tumor” that does not trigger a strong immune response into a “hot tumor” that does, which would enhance the efficacy of immune checkpoint inhibitor therapies that amp up our natural defenses against cancer
- Interfere with cytokine pathways to reduce the accumulation of certain immune cells in the TME that aid tumor development
- Eliminate or reduce the population of regulatory T-cells (Tregs) that suppress the immune system response
- Activate and boost poorly performing T-cells
- Change conditions within malignant cells that help T-cells better recognize and eliminate tumor cells that have not responded to treatment.
Scientists need to understand how the rest of the body influences the TME and impacts cancer progression. This includes a patient’s gastrointestinal microbiome as well as a person’s diet, metabolism, exercise and underlying conditions that may affect treatment response, according to an April 2021 report in the American Association for Cancer Research (AACR) journal Cancer Discovery.
“The clinical approval of drugs and cell-based therapies directed toward the blood vasculature, immune checkpoints, and T-cells has driven the continued exploration of the TME for additional targets to exploit,” the report said.
“It will be critical to move beyond the current focus on targeting individual cell types of interest and rather adopt a more comprehensive systems-level approach in which we analyze and integrate all TME components to identify and disable the critical nodes.”
If you’ve been diagnosed with cancer and are interested in a second opinion about your diagnosis or treatment plan, call us or chat online with a member of our team.