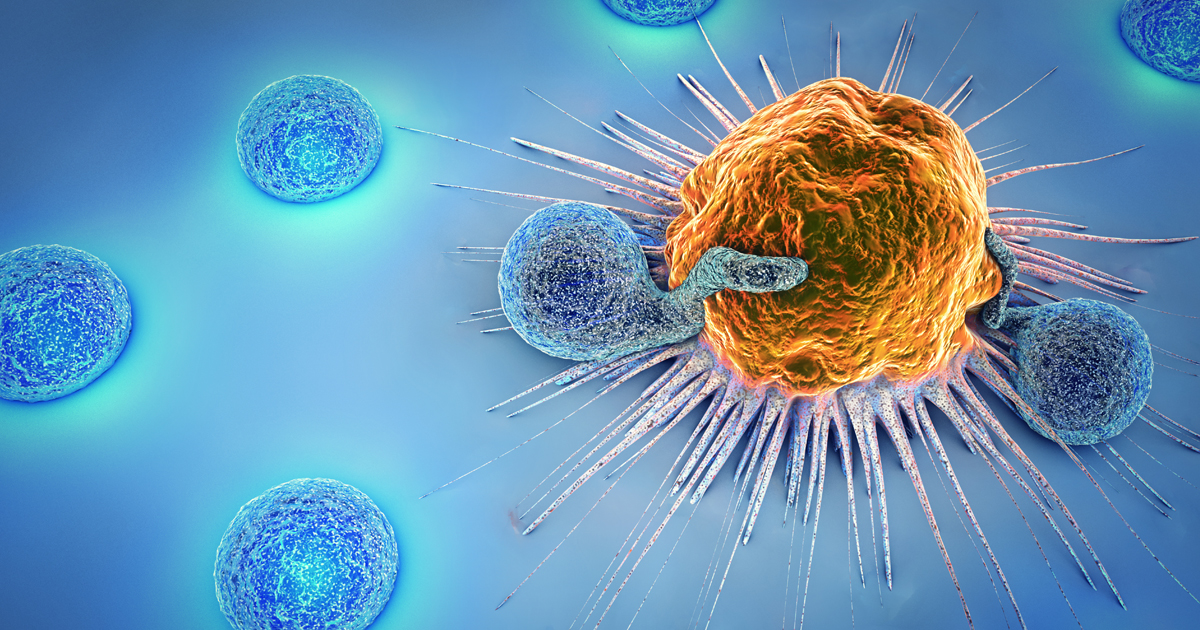
One law of physics says that for every action, there is an equal and opposite reaction. And while Isaac Newton's third law of motion doesn't exactly apply to the immune system, it is this basic principle that keeps our T-cells in check. That balance is struck thanks to immune cells called regulatory T-cells, or T-regs. "They're like an off switch," says Alan Tan, MD, Medical Oncologist at our hospital near Phoenix. "Once your T-cells have fought off a pathogen, you need something to regulate the immune response—to turn it off." Regulatory T-cells are critical in preventing autoimmune disease, by stopping the body from attacking itself and helping to keep it in healthy working order.
Using the off switch
But researchers have discovered that sometimes, cancer cells take advantage of this off switch, recruiting armies of T-regs to protect them from the immune system. In fact, identifying T-regs in tumors often means those patients can expect poor outcomes, research shows. "T-regs are involved in maintaining a working immune system and protecting us from developing autoimmune disease and allergies," Dr. Tan says. "From a cancer standpoint, however, they can help tumors grow by suppressing an effective immune response."
“ T-regs are involved in maintaining a working immune system and protecting us from developing autoimmune disease and allergies. From a cancer standpoint, however, they can help tumors grow by suppressing an effective immune response.” - Alan Tan, MD, Medical Oncologist
T-cells are members of the adaptive immune family. Unlike innate immune cells, which automatically attack viruses and bacteria, adaptive immune cells adjust over time to specific threats, attacking pathogens and remembering them should they attack again. T-cells are also critical players in immunotherapy cancer treatments. Drugs known as checkpoint inhibitors allow T-cells to better recognize and attack cancer cells. And CAR T-cell therapy, recently approved for some blood cancers, uses a patient’s re-engineered T-cells to attack cancer.
The various types of T-cells protect the body in different ways:
- Killer T-cells, also called cytotoxic cells, kill damaged cells or those that have been infected by a virus.
- Helper T-cells support various aspects of an immune response, stimulating B-cells to make antibodies and helping killer T-cells develop.
- Memory T-cells recognize antigens they’ve previously attacked. These are the cells vaccines use to recognize specific viruses, such as measles or polio.
- Natural killer T-cells, which are different than killer T-cells, are hybrids, launching an initial attack like an innate immune cell, but also remembering and recognizing certain viruses like an adaptive immune cell.
How do regulatory T-cells work?
Regulatory T-cells work differently than all those above. When functioning properly, T-regs kick in just as an immune response is winding down. Like chaperones at a school dance, they turn on the lights when the party is over and clear out the hall. If not for T-regs, the immune system would run amok and start attacking healthy cells and organs. Malfunctioning T-regs have been linked to a range of diseases, including diabetes and arthritis. "Lupus is a classic example of regulatory T-cell dysfunction," Dr. Tan says. "We all need that off switch so we don’t have too much immune stimulation."
Learn more about the connection between autoimmune diseases, like Lupus, and the connection to cancer.
Scientists in 2003 found evidence that melanoma cells may secrete a substance called heavy-chain ferritin, or H-Ferritin, that may activate regulatory T-cells to protect tumors from the immune system. In a 2004 article published in Nature Medicine, researchers suggest that ovarian tumor cells are able to recruit regulatory T-cells, describing their presence as a "smoking gun" that "predicts a marked reduction in patient survival." And a paper published in April in The Journal of Immunology, discusses the prevalence of T-regs in aggressive breast cancer and tumors, concluding that "invasive cancer in humans is associated with an expansion of T-regs that suppress a tumor-specific immune response."
In an article published in January, researchers in Austria suggest that targeting regulatory T-cells may prove promising for new immunotherapy treatments or in improving the outcomes of patients taking existing immunotherapy drugs. But, experts say, they should be treated with caution. Because T-regs are primarily responsible for preventing autoimmune diseases, depleting them to help fight cancer may produce devastating side effects. For instance, one strategy being explored targets a molecule called CCR8, which is found on T-regs inside tumors. But CCR8 is also found in cardiac muscle and in the liver. So targeting those cells may cause serious immune-related problems in those organs.
Still, Dr. Tan says, reducing the T-reg population in cancers remains a promising area of immunotherapy research. "The existence of regulatory T-cells in the tumor microenvironment is a major obstacle to improving the outcomes for cancer patients taking immunotherapy," he says. "If we could selectively deplete tumor-infiltrating T-regs, then we may be able to unleash potent anti-tumor responses."
Learn why immunotherapy may work for some patients but not others.