Of the many types of prostate cancer, prostatic adenocarcinoma is by far the most common type and is diagnosed in up to 99 percent of prostatic cancer cases. It develops in the gland cells that make prostate fluid.
Prostate cancer is second only to skin cancer as the most common cancer in men in the United States. When diagnosed in early stages, prostate cancer is highly treatable. The risk of prostate cancer increases with age. Other risk factors include obesity, diets high in saturated fats or a family history of prostate cancer. African-American men are at high risk of developing prostate cancer—they are 70 percent more likely to get the disease than non-Hispanic Caucasians.
At City of Hope, our oncology staff has prostate cancer experts who develop a comprehensive treatment plan tailored specifically for each patient. Your cancer care plan will include evidence-based medical treatments and technologies, along with supportive care services to help reduce side effects and keep you strong in body, mind and spirit.
About the prostate and prostate cancer
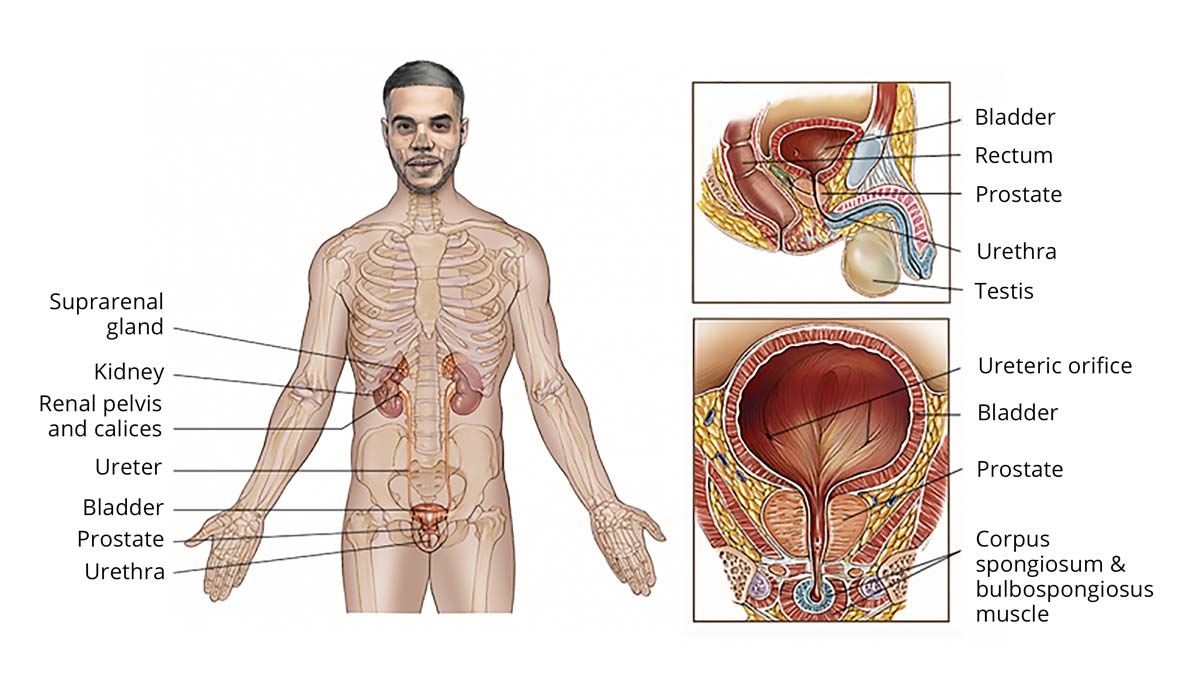
The prostate gland is part of the male reproductive system and produces fluid that mixes with semen during ejaculation to help sperm travel. The prostate is a walnut-sized, rubbery organ that surrounds the urethra—the urinary duct that carries urine from the bladder out of the body—and sits directly below the bladder.
The prostate gland, which grows during puberty, is considered an organ and is made up of several dozen lobules or saclike glands, held together with connective prostate tissue and muscle between them. The glands are called exocrine glands, because they secrete liquid to outside the body.
An enlarged prostate, called benign prostatic hyperplasia (BPH), is common in men over the age of 40 and may obstruct the urinary tract. The abnormal prostate cell growth in BPH is not cancerous and doesn’t increase your risk of getting prostate cancer. However, symptoms for BPH and prostate cancer can be similar.
A condition called prostatic intraepithelial neoplasia (PIN), where prostate gland cells look abnormal when examined under a microscope, may be connected to an increased risk of prostate cancer. Prostate cancer is often caught by a doctor performing a digital rectal exam (DRE), through a prostate-specific antigen (PSA) blood test, through a prostate biopsy or with a CT scan.
Another condition, prostatitis, is the inflammation of the prostate. While not cancerous, it may cause higher PSA levels in the blood.
When prostate cancer is found, pathologists stage the disease using a Gleason score, which grades the extent and arrangement of the cell mutations. For instance, a Gleason score of 6, the lowest possible, indicates a low-grade tumor, while cancers with scores of 9 or 10 are considered high-grade or the most aggressive and most likely to spread.
Types of prostate cancer
Adenocarcinoma of the prostate
Adenocarcinomas may occur almost anywhere in the body. They form in the glandular epithelial cells that line the insides of the organs and secrete mucus, digestive juices or other fluids. In the prostate, adenocarcinoma is also called glandular prostate cancer.
Symptoms of adenocarcinoma of the prostate may include a frequent urge to urinate, painful urination and ejaculation, and blood in the semen. Treatment options may start with active surveillance of the cancer, which generally grows very slowly. Treatments may include surgery, chemotherapy, radiation therapy, immunotherapy or hormone therapy. A radical prostatectomy, which is a surgical procedure to remove the prostate, may be an option when the cancer is limited to the prostate.
Some side effects of treatment may include urinary problems or erectile dysfunction.
Main subtypes of adenocarcinoma of the prostate
Acinar adenocarcinoma (conventional adenocarcinoma): This cancer accounts for virtually all prostatic adenocarcinomas. Acini cells line the prostate’s fluid-secreting glands. The cancer starts growing in the back (periphery) of the prostate near the rectum and may be felt during a doctor’s digital rectal exam. The disease increases PSA levels.
Prostatic ductal adenocarcinoma (PDA): This cancer is a rarer but more aggressive form of adenocarcinoma. It develops in the cells lining the tubes and ducts of the prostate gland. When it occurs, it frequently develops along with acinar adenocarcinoma. This cancer type doesn’t necessarily increase PSA levels, making it harder to detect.
Other types of prostate cancer
There are many other prostate cancers, but they are incredibly rare given the overwhelming diagnoses of prostatic adenocarcinomas. Some of these other cancers include:
- Transitional cell carcinoma, or urothelial cancer, which may either start in the urethra or bladder and spread to the prostate or, very rarely, vice-versa
- Neuroendocrine tumors, or carcinoids, which don’t produce PSA, appearing in the nerve and gland cells that make and release hormones into the bloodstream
- Small cell carcinoma, the most aggressive type of neuroendocrine cancer in the prostate that develops in small round cells of the neuroendocrine system
- Squamous cell carcinoma, a very rare, fast-growing form of prostate cancer that starts in the flat cells that cover the prostate glands
- Prostate sarcoma (also called soft-tissue prostate cancer), which develops outside the prostate glands in the soft tissue—the muscle and nerves—of the prostate
When prostate cancer reappears
Prostate cancer may show up elsewhere in the body or—after treatment—reappear in the prostate or elsewhere. These cancers are:
Recurrent prostate cancer: This is a cancer that returns to the prostate after treatment. It’s also called a local recurrence. Prostate cancer treatment is designed to kill cancerous cells, but it may leave some undetected cells behind.
Metastatic prostate cancer: This is prostate cancer that spreads to other parts of the body. These cancer cells may have traveled via the bloodstream or the lymphatic system. A metastasis of the original prostate cancer is also called a regional recurrence or distant recurrence.
Because most prostate cancer cells are less aggressive and slower growing than cells found in many other cancers, about 90 percent of prostate tumors are diagnosed before the cancer has had a chance to spread outside the prostate region. If the cancer metastasizes, making it an advanced prostate cancer, it most likely will develop in nearby tissue, lymph nodes or seminal vesicles first before traveling to the bones or to the liver, lungs, brain, more distant lymph nodes or other organs.