Remarkable progress in blood cancer treatments in recent years has significantly increased survivability rates for these hard-to-treat cancers, aided in large part by major advances in the fields of immunotherapy and targeted therapy.
Blood cancer treatment breakthroughs have also used existing drugs in new combinations and for new treatments, while other advances have come from using them in new regimens or at different dosing levels. Unlike solid tumors that mass in organs or other areas of the body, blood cancers are liquid tumors that circulate in the bloodstream.
Among the various types of blood cancers, the National Cancer Institute says five-year survivability has increased from 1990 to 2018, from:
- 45 percent to 65.7 percent for leukemia
- 51 percent to 73.8 percent for non-Hodgkin lymphoma
- 29 percent to 57.9 percent for multiple myeloma
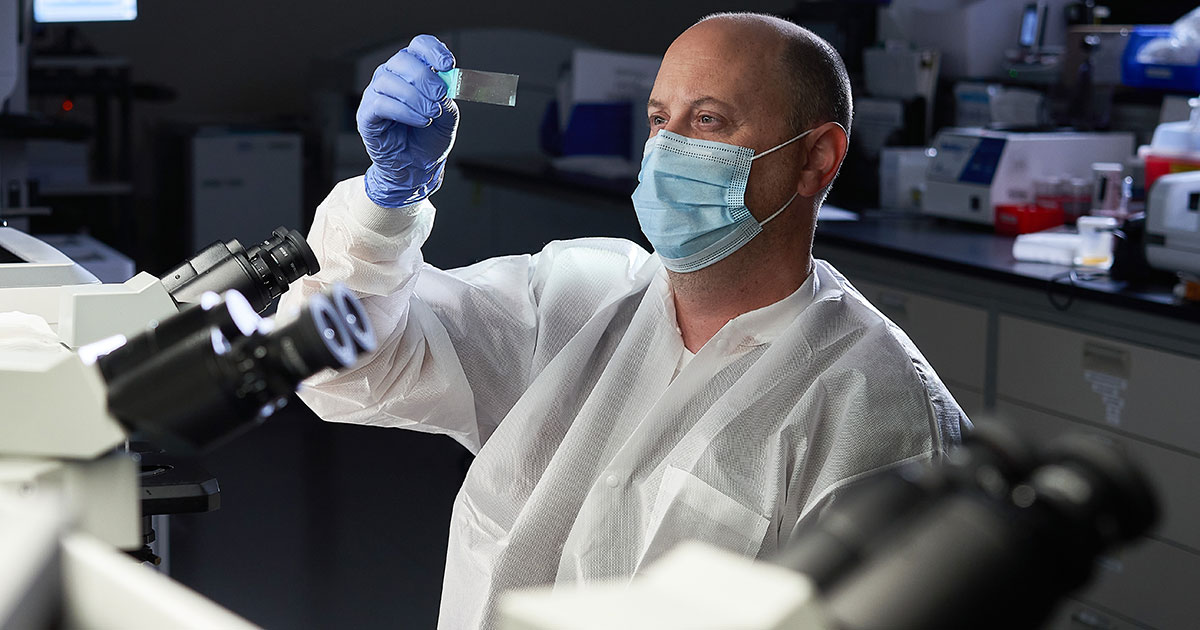
“There have been dramatic changes in treating hematologic malignancies, more than for any other cancers, over the last five years,” says Jeffrey R. Schriber, MD, Director of Hematologic Malignancies at City of Hope Phoenix. “Many of the recent changes in oncology have occurred first in hematologic malignancies, and virtually every single major hematologic malignancy has undergone major changes in treatment over the past five to 10 years.”
Chimeric antigen receptor (CAR) T-cell therapy, antibody-drug conjugates (ADCs) and bispecific antibodies, for instance, are having an impact on treating cancer patients with multiple myeloma, which is a plasma cell cancer. In 2022 alone, the U.S. Food and Drug Administration (FDA) approved three new drugs to treat multiple myeloma.
The FDA also gave “Breakthrough Therapy Designation” in November to the drug elranatamab to treat multiple myeloma. The designation, given to drugs that show early clinical evidence of providing substantial improvement over existing therapies in the treatment of serious or life-threatening diseases, may help expedite the drug’s development and review process.
In this article, we’ll explore several types of treatment for blood cancers, including:
- Immunotherapy
- CAR T-cell therapy
- Minimum residual disease testing
- Targeted therapy
- Stem cell transplantation
We’ll also explore ongoing research for new cancer treatments.
If you’ve been diagnosed with leukemia or another blood cancer, such as lymphoma or multiple myeloma, and are interested in a second opinion about your diagnosis and treatment plan, call us or chat online with a member of our team.

Immunotherapy for blood cancer
Cancer cells have a knack for evading the immune system’s attempts to rid the body of foreign or harmful cells. They divide rapidly and mutate frequently, making it harder for the immune system to find and destroy them.
Over the years, chemotherapy has been the first-line treatment for blood cancers. But chemotherapy drugs may be toxic and often take a heavy physical toll on cancer patients because, while they attack fast-growing cancerous cells in the body, they also attack non-cancerous ones.
Immunotherapy drugs, on the other hand, are designed to stimulate the immune system to do a better job of eliminating cancer cells in a way that spares healthy cells.
Immunotherapy cancer treatment makes it easier for the immune system to spot cancer cells and trigger an immune attack. Immunotherapy drugs may be used by themselves or in conjunction with chemotherapy, radiation therapy and/or other treatments.
CAR T-cell therapy
T-cells are white blood cells, which are part of the immune system and help destroy foreign cells. At the cutting edge of immunotherapy for hematologic cancers is an approach designed to take prime advantage of these killer cells: CAR T-cell therapy.
In CAR T-cell therapy, infection-fighting T-cells are taken from the patient through apheresis, which uses a procedure similar to what’s used to when people donate blood. With CAR T-cell therapy, however, the process is more complex: The blood is removed from the patient, filtered to extract T-cells, then returned to the patient’s bloodstream. The extracted T-cells are modified in a laboratory into CAR T-cells to better attack the cancer, then multiplied before being infused back into the patient’s body.
Some CAR T-cell therapy drugs for blood cancers are designed to recognize and bind to the B-cell maturation antigen (BCMA) that is found on almost all multiple myeloma cells, leading to their destruction. Others may attach to CD19 proteins on the surface of the cancer cells, allowing the modified T-cells to attack and kill the cancer cells.
Research published in February in the journal Nature shows some promising CAR T-cell treatment developments for chronic lymphocytic leukemia (CLL)—a slow-growing cancer that develops mostly in the blood and bone marrow. Two CLL patients given CAR T-cell therapy later had no evidence of disease and had detectable, working CAR T-cells a decade after therapy.
Despite the progress, hurdles persist in improving the viability of CAR T-cell therapy in treating cancer.
“It’s a complicated process,” Dr. Schriber says. First, you have to collect the T-cells from the patient. They get shipped to be manufactured to be able to target the cancer. It’s a four-to-six-week process that isn’t always successful. And during that time, we have to find ways to control the disease in patients who are not responding to other treatments.”
CAR T-cell therapy also has potentially life-threatening side effects. Some of those therapies are only available under restricted programs called Risk Evaluation and Mitigation Strategy (REMS). The FDA says it may require REMS for certain medications “to help ensure the benefits of the medication outweigh its risks.”
Major potential complications of CAR T-cell therapy are cytokine release syndrome (CRS) and immune effector cell associated neurotoxicity syndrome (ICANS), both of which may be life-threatening.
The CAR T-cell treatments may cause a large, rapid release of immune substances called cytokines into the bloodstream, which the NCI says may lead to fever, nausea, headache, rash, rapid heartbeat, low blood pressure and trouble breathing.
Symptoms of ICANS include headache, confusion, delirium and seizures.
Minimum residual disease testing
Minimal residual disease (MRD) testing, or measurable residual disease testing, allows oncologists to measure the amount of cancer cells present at the molecular level following cancer treatment. Monitoring this aspect of the disease may help doctors determine how well a treatment is working and whether maintenance therapy is needed.
MRD testing, which helps measure the success of primary treatments, is used as an indicator of likely cancer recurrence in blood cancer patients, Dr. Schriber says. An MRD-negative patient shows no detectable signs of cancer following treatment. MRD positive means cancer cells have been detected. Patients who are MRD positive should talk to their doctor about potential next steps. Progress continues in efforts to develop more sensitive testing in order to detect the presence of even the smallest amounts of residual cancer cells.
Targeted therapy
Kinases are enzymes that help regulate cellular activity. Among them are tyrosine kinases, which regulate cell growth and division. Some targeted therapy drugs called tyrosine kinase inhibitors are designed to disrupt specific cell signaling that may lead to some blood cancers. Key targets of these inhibitors are Bruton’s tyrosine kinase (BTK), which may cause malignant B-cells to proliferate. BTK inhibitors are designed to stop this type of signaling.
BTK inhibitors used in the treatment of certain leukemias have been gaining traction as an alternative to chemotherapy since they first came on the market in 2013. A half-dozen tyrosine kinase inhibitors are being used to treat chronic myeloid leukemia (CML), targeting the BCR-ABL protein that makes CML cells grow and reproduce uncontrollably. However, because these drugs do not make the leukemia go away permanently, they need to be taken on a continuing basis.
Targeted therapy also includes drugs that link monoclonal antibodies with cytotoxic agents, bringing the concentrated chemotherapeutic agent directly to targeted cancer cells.
Stem cell transplantation
Transplanting blood stem cells, also called hematopoietic stem cells, involves infusing healthy stem cells into the body to stimulate new bone marrow growth, suppress disease and reduce the possibility of relapse. A transplant using the patient’s own stem cells, called an autologous stem cell transplant, may be performed for most types of multiple myeloma and some lymphomas, says Roy Thomas, Director of Operations for Hematology and Stem Cell Transplants at City of Hope Chicago.
A transplant using stem cells from a relative or an unrelated donor, called an allogeneic stem cell transplant, may be used for cancer patients with leukemia, certain types of lymphoma and some high-risk multiple myeloma, Thomas says.
Research is ongoing to find more effective ways to produce the blood stem cells needed for transplantation. A Cedars-Sinai study, published in the journal Blood in January 2022, found that stem cells that express the protein syndecan-2 on their surface were better at reproducing than those that didn’t. The study concluded that using only syndecan-2 stem cells may lead to better and less toxic transplants than using stem cells that don’t express syndecan-2.
Ongoing research for new cancer treatments
Much more progress is expected in the field of blood cancer research in the coming years as clinical trials continue to explore many more aspects of the diseases. This includes research into new areas, such as how tumor cells relate to the tumor microenvironment (TME), which is made up of stromal cells and extracellular matrix. A study published in the August 2021 issue of Journal of Hematology & Oncology says “targeting TME components is expected to provide novel insights for the precise treatment of B-cell lymphoma.”
In the area of targeted therapy, research is studying a less-aggressive cancer called myelodysplastic syndrome (MDS), which may eventually progress to acute myeloid leukemia (AML), the most common type of acute leukemia in adults that may cause a buildup of abnormal red blood cells, white blood cells or platelets. Some of the research is studying histone deacetylase (HDAC) inhibitors and other potential drugs that affect how genes are turned on and off in the two diseases.
In its efforts to make groundbreaking research available to its patients, City of Hope leads in a number of blood cancer clinical trials at various locations. Clinical trials often offer qualifying patients treatment options that may not be otherwise available.
If you’ve been diagnosed with leukemia or another blood cancer, such as lymphoma or multiple myeloma, and are interested in a second opinion about your diagnosis and treatment plan, call us or chat online with a member of our team.