It’s not hard to imagine organisms inside your digestive system upsetting your stomach, making you nauseous or causing bouts of diarrhea. But what if, in certain situations, the bacteria that swim in your colon are being altered in ways that impair your memory or thinking abilities, make you depressed or cause insomnia? While scientists have known that gut bacteria have co-existed with humans for thousands of years, they may be affecting us in ways we’re only just beginning to realize.
For cancer patients, chemotherapy treatments may be altering the body’s normal balance of bacteria in ways that produce the forgetfulness known as “chemo brain” or “chemo fog.” Imbalances in gut bacteria may contribute to patients’ fatigue or lead to severe pain because of its effects on the nervous system. Some gut organisms are also believed to promote tumor growth, raising other concerns about the role they may play in cancer.
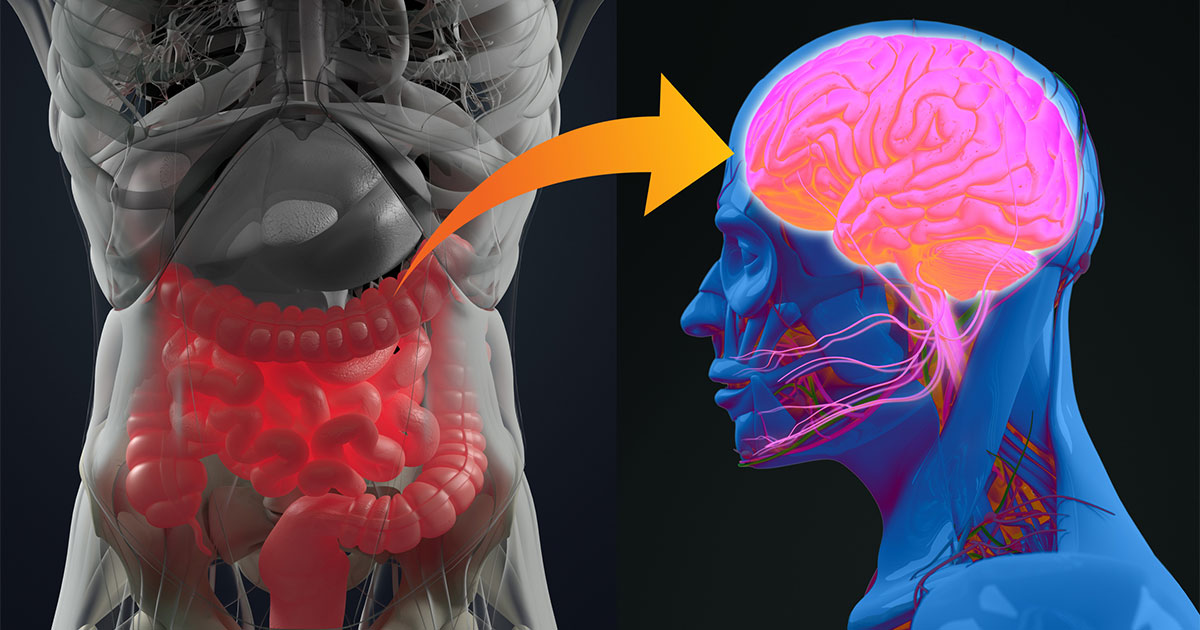
Research investigating these possibilities stems from the growing knowledge of the gut-brain axis, a two-way highway inside the body where organisms in the digestive system are sometimes able to hitch a ride via the circulatory system and impact cognitive function.
“You have millions of bacteria in your colon, but they don’t get into your blood circulation because of the integrity of the lining of the colon. The cells in your colon are so tightly packed next to one another that the bacteria cannot penetrate between the cells,” says Pankaj Vashi, MD, Vice Chief of Staff and Medical Director of Gastroenterology/Nutrition & Metabolic Support at Cancer Treatment Centers of America® (CTCA), Chicago. “It’s been shown if you have bad bacteria in your colon, it actually impairs the tight integrity of the colon to a point where bacteria can migrate between cells into your blood circulation, which can go to the brain and cross the blood-brain barrier.”
In this article, we’ll answer these questions:
- What is the gut microbiome?
- What is the gut-brain axis?
- Is bacterial imbalance connected to neurological diseases?
- Why do some researchers think there may be a connection to chemo brain?
- Should you be taking probiotics?
If you’ve been diagnosed with cancer and want to learn more about treatment options at CTCA®, or you’re interested in a second opinion on your cancer diagnosis and treatment plan call us or chat online with a member of our team.
What is the gut microbiome?
Literally trillions of bacteria, representing hundreds of different species, are swimming around inside the body. Those in the digestive system are known by a number of terms, such as gut microbiota, gut flora or microbiome. These bacteria are generally divided into good bacteria, or those that promote good health and help fight infections, and bad bacteria, which can cause infection or disease.
Most of these bacteria live in the large intestine, while others live in the small intestine or stomach. There’s no optimal balance of bacteria that’s beneficial for all people. Instead, the balance will be affected by a person’s age, diet, local environment and his or her own genetic make-up. Also, the distinction between good and bad bacteria may blur, sometimes changing as a result of a particular strain or its location in the digestive system.
What is the gut-brain axis?
Millions of neurons in the brain and the digestive system are connected through pathways in the nervous system, such as the vagus nerve, a critical transmission line in what’s called the parasympathetic nervous system. Vagus nerves carry cell signals that connect the brain, heart and digestive system and help regulate heart rhythm, digestion, immune response and other bodily functions.
“We know that bad bacteria produce toxins, metabolites, neural hormones that impact your gut-brain tract,” Dr. Vashi says.
Some of the neurotransmitters in the brain that control feelings and emotions are also produced in the gut. One of these neurotransmitters, for instance, is serotonin, which helps improve mood.
A bacterial imbalance in the digestive system could reduce serotonin levels and elevate anxiety levels.
Is bacterial imbalance connected to neurological diseases?
The implications of the study into the gut-brain connection have led to theories that the microbiome may be a factor in neurological disorders such as Parkinson’s disease, Alzheimer’s disease, multiple sclerosis and strokes.
“We know the gut microbiome plays a major role in certain neurological conditions,” Dr. Vashi says. “There’s also some association between depression and eating habits that explains the obesity that goes along with the gut microbiome.”
A 2016 study found that people with Alzheimer’s disease who were given probiotics showed moderate improvements to their memory and thinking skills. The study involved individuals taking a daily dose of probiotics lactobacillus and bifidobacterium bacteria for a 12-week period.
Why do some researchers think there may be a connection to chemo brain?
When it comes to addressing chemo brain, researchers have to first document the specific symptoms of the condition. Many times, the cognitive impairments are self-reported by patients, not behaviors or experiences researchers can observe clinically.
“We really don’t know what chemo brain is. We don’t know what it means. It means you get forgetful, but we don’t know if it’s the chronic effect of being on chemo, or whether it has any relationship with the gut microbiome,” Dr. Vashi says. “It’s not like patients who have great gut microbiome before they start chemo will be less likely to get chemo brain versus those who do not. That kind of prospective study has not been done.”
The chemo brain diagnosis is usually connected to people experiencing a range of symptoms, sometimes involving perception, language, attention and memory, other times involving reasoning and problem-solving impairments. Some cancer patients experience symptoms even before their treatment starts.
“While CRCI [cancer-related cognitive impairment] has been associated with various treatment modalities, including radiotherapy, chemotherapy, hormone therapy and novel systemic therapies, it has been also detected prior to cancer treatment. Therefore, the effects of cancer itself with or without the psychological distress may be involved in the pathogenesis of CRCI as a result of altered coping mechanisms after cancer diagnosis,” scientists from Comenius University in Slovakia wrote in a December 2021 review.
The review suggests that the gut microbiome may influence brain function through short-chain fatty acids (SCFAs), which are produced by beneficial bacteria when fiber is fermented in the colon. The SCFAs provide energy to colon-lining cells.
Human studies have been insufficient to support the connection between the gut microbiome and chemo brain, Dr. Vashi says, adding, “It’s too early to say that, but there are some animal studies that suggest that.”
For example, a 2021 study on mice showed chemotherapy may lead to dysbiosis, a disruption and imbalance of gut flora, which was “associated with cognitive impairment, anxiety, and mood disorders.”
Should you take probiotics?
If they can find a relationship between the gut bacteria and chemo brain, researchers say probiotics and prebiotics may be helpful in promoting bacteria that helps improve symptoms. Because probiotics are good for you, Dr. Vashi says it makes sense to make sure you’re getting plenty of those foods in your diet—even if other proposed benefits haven’t been scientifically proven.
“I’d take them. There is really no downside. It helps your digestive tract. It’s good for you,” Dr. Vashi says, suggesting people get their prebiotics and probiotics by eating foods that are chock full of them.
“I think people forget—and this is typically an American and Western society tendency that I get a little disappointed with—they want to fix everything with a pill. I come across patients who don’t want to watch their diet, don’t want to watch their weight, but they still want to take multivitamins and vitamin D and probiotics and all that stuff,” Dr. Vashi says.
“Getting your probiotics naturally is the way to go. That way, you’re not only getting your prebiotics and probiotics, but you also get many other nutrients,” he says. “You get a lot of antioxidants. You get vitamin C if you’re eating citrus fruits. So, you get a lot of other stuff you won’t get just by taking pills.”
If you’ve been diagnosed with cancer and want to learn more about treatment options at CTCA®, or you’re interested in a second opinion on your cancer diagnosis and treatment plan, call us or chat online with a member of our team.