A woman’s ovaries, fallopian tubes and peritoneum are located in the same vicinity, and each serves a different but related function in the reproductive process and the production of hormones. Like other body parts, these organs also may develop cancer. In fact, ovarian, fallopian tube and primary peritoneal cancers are the most common cause of death in women with cancer of the reproductive system.
So, what’s the difference between ovarian, fallopian tube and peritoneal cancers? It turns out, not much. In fact, cancer that forms in any of these organs is referred to as ovarian cancer and is treated nearly identically. Recent research indicates that the most common form of ovarian cancer—high-grade serous ovarian carcinomas—may begin most often in the fallopian tubes and spread to the ovaries long before the cancer is diagnosed. These findings may help explain why many ovarian cancers are not diagnosed until later stages and may help science find ways to detect the disease earlier and develop new prophylactic strategies, especially for women at high risk.
The research also is an example of the advances made in better understanding the origins of ovarian cancer and how to produce better outcomes in treating it, says Julian Schink, MD, Chief Medical Officer for Cancer Treatment Centers of America® (CTCA) and Chief of the Division of Gynecologic Oncology at CTCA® Chicago. “Our understanding of the disease has improved dramatically,” he says.
| What they do? |
|---|
| The ovaries are located at each side of the uterus. Each of the two ovaries is about 1.5 inches in size. The ovaries are the primary source of estrogen and progesterone and affect breast size, body hair, menstrual cycles, pregnancy and body shape. During and after menopause, the ovaries stop releasing eggs and creating specific types of hormones. |
| The fallopian tubes connect the ovaries to the uterus, the organ in the pelvic area that carries a fetus during pregnancy. Each woman typically has two fallopian tubes, which are located on each side of the uterus. During a woman's monthly menstrual cycle, one of the ovaries releases an egg, which travels to the uterus through a fallopian tube. |
| The peritoneum lines the abdomen and other abdominal organs, such as the bladder, rectum and the ovaries and fallopian tubes. This tissue is covered by a peritoneal fluid that allows the organs to move around one another in the abdomen. Peritoneal cancers are very rare. |
A challenging diagnosis
Like some other challenging cancers, such as lung cancer and pancreatic cancer, symptoms in the early stages of ovarian cancer are subtle and may be ignored or misinterpreted as other common ailments. In the words of Dr Schink: “Ovarian cancer symptoms don’t shout, they whisper”. Only about 20 percent of ovarian cancers are diagnosed early, when the disease may be easier to treat. In most cases, ovarian cancer patients are diagnosed after the disease has progressed to stage 3 or stage 4.
Compounding the challenge, no reliable diagnostic tools are currently available to help detect ovarian cancer early. Regular gynecologic exams, including a Pap smear, may help identify precancerous cells or early-stage cervical cancer, but they do not detect early ovarian cancer.
Some women may experience symptoms of ovarian cancer, but in many cases, they mimic symptoms of other conditions, such as digestive issues. Some symptoms may be linked to ovarian cysts, which are typically not cancerous.
Symptoms of ovarian cancer include:
- Bloating
- Pelvic or abdominal pain
- Early satiety (feeling full quickly) or difficulty eating
- A need to urinate frequently or urgently
- Back pain
- Fatigue
- Pain during sex
- Menstrual changes
Monitoring risk factors
Women who have inherited mutations in their BRCA1 or BRCA2 genes are more likely to develop ovarian cancer. Other risk factors for ovarian cancer include:
Age: More than 70 percent of new cases are diagnosed in women 55 and older.
Endometriosis: This is a painful condition in which the endometrium (the lining of the uterus) grows outside the uterine cavity.
Fertility issues: Women who have difficulty trying to conceive, use fertility drugs or treatments or give birth after the age or 35 may be at higher risk. Conversely, women who give birth before the age of 26 may have a lower risk.
Family history: Besides having an inherited BRCA gene mutation, a family history of ovarian, breast and colorectal cancer may indicate higher risk. Several inherited cancer syndromes also are linked to a risk of ovarian cancer.
Obesity: Being overweight has been linked to higher risk of many cancers. It may also reduce the effectiveness of some cancer therapies and has been linked to poorer treatment outcomes.
Some women with risk factors, especially mutated BRCA genes, may choose to have prophylactic surgery to remove their ovaries before cancer has a chance to develop. Researchers say, however, that if further research supports the theory that some ovarian cancers begin in the fallopian tubes, it “could result in a major change in the way we manage this disease for patients at risk.” Theoretically, removing the fallopian tubes and preserving the ovaries may result in better long-term health benefits for many women.
Improved treatment options
Because it’s often diagnosed in advanced stages, ovarian cancer may be difficult to treat. The five-year survival rate for a patient diagnosed with ovarian cancer is less than 50 percent. Common treatments for ovarian cancer include:
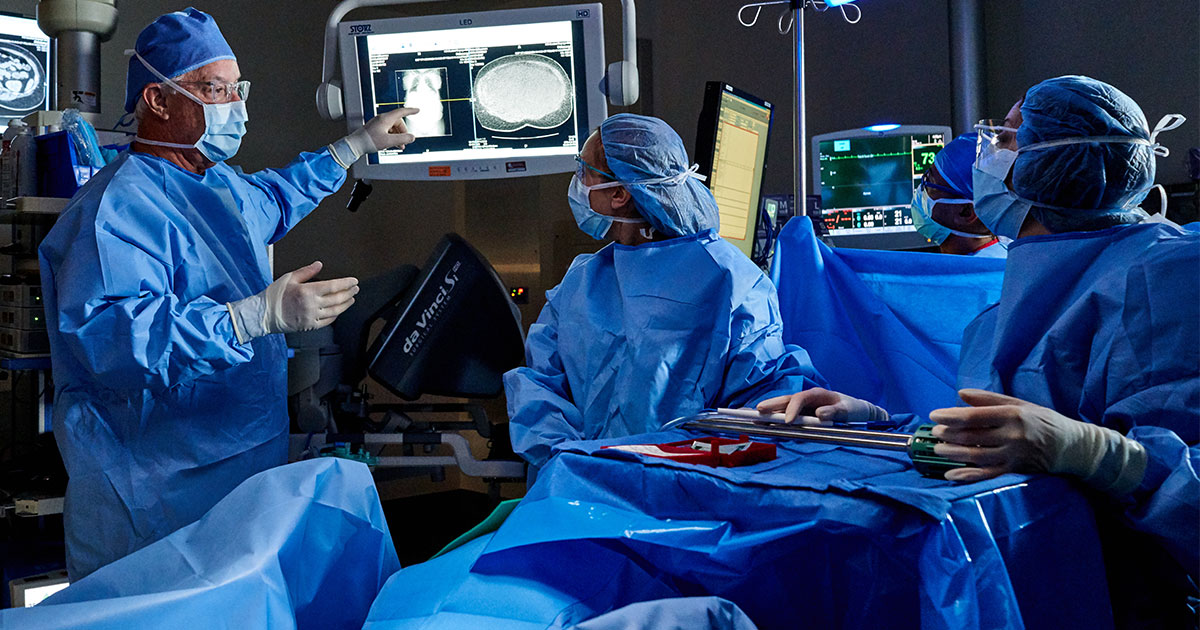
- Surgery
- Chemotherapy
- Radiation therapy
- Hormone therapy
But in recent years, new treatments have led to better outcomes. Specifically, targeted therapy drugs called PARP inhibitors have improved outcomes for many patients. First approved in 2014, PARP inhibitors target a protein called poly ADP-ribose polymerase, or PARP, which monitor damage to DNA in cells. PARP proteins are kind of like the cell’s 911 call center, receiving signals of faulty DNA and summoning genes to repair the damage. PARP inhibitors work by short-circuiting those signals and disrupting the repair process in cancer cells, which may cause them to die.
“Our treatment options have improved significantly—with more effective drugs, targeted therapies, a broader array of treatments, newer drugs like PARP inhibitors—and that’s significantly improving people’s lives,” Dr. Schink says. “Those are really exciting developments that have happened over the course of my career.”

