Immune system failures are behind many cancers, allowing tumors to grow unchecked. Sometimes the cancer cells may:
- Mimic healthy cells, disguising them from disease-fighting immune cells
- Successfully turn off the body’s natural immune response
- Use immune cells to help them grow
Immunotherapy is a type of treatment developed to overcome such immune system deficiencies.
Getting the immune system to do its job has been particularly difficult when it comes to fighting breast cancer. While immunotherapy has become a promising treatment against many cancers, it’s only recently gained traction in fighting breast cancer.
“Immunotherapy for breast cancer has significantly improved over the last few years. The hard part is waiting for the overall survival data, which takes years,” says Laura C. Farrington, DO, Medical Oncologist at Cancer Treatment Centers of America® (CTCA), Chicago.
The U.S. Food and Drug Administration (FDA) approved the first breast cancer immunotherapy treatment in March 2019 and a second in November 2020, both for patients with advanced or metastatic triple-negative breast cancer (TNBC). The treatments are delivered in combination with certain chemotherapy drugs.
Targeted therapy—which, like immunotherapy, is a field of precision medicine—has yielded many more new breast cancer treatments. The advocacy site breastcancer.org, for instance, lists 18 targeted therapies—using lab-created antibodies or antibody drugs—approved to treat various forms of breast cancer, compared to the two immunotherapies approved so far. Still, many scientists see immunotherapy treatments for breast cancer as a promising field of research.
Breast cancer’s ‘cold’ tumor problem
“Our immune system is very complex. There’s a lot of emerging research trying to figure out why some cancers do not respond to immunotherapy," Dr. Farrington says.
Breast cancer tumors, like many solid tumors affecting other parts of the body, frequently contain few of the immunological cells immunotherapy drugs use when kicking into action. A National Institute of Health study describes these as “cold” tumors and says “cancers that are classically immunologically cold” include most breast cancers, as well as glioblastomas, ovarian cancer, prostate cancer and pancreatic cancer.
Breast cancer tumors typically have fewer tumor-infiltrating lymphocytes (TILs), such as T-cells, than other cancers. Studies have shown that the larger the concentration of TILs in a breast cancer tumor, the better the prognosis for a positive outcome from treatment.
Many solid tumors such as those found in various breast cancers have immune cells that aren’t working to kill the tumor cells—in fact, they’re actually feeding them, helping them grow.
Checkpoint inhibitors
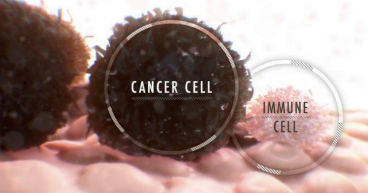
Both approved immunotherapy drugs for breast cancer rely on proteins called immune checkpoint inhibitors.
One function of the immune system is to keep itself from attacking healthy cells in the body. It does this by using “checkpoints,” which the American Cancer Society describes as “proteins on immune cells that need to be turned on (or off) to start an immune response.” Some breast cancer cells are able to use these checkpoints to avoid an immune system attack.
That’s where checkpoint inhibitors come into play. These drugs target the checkpoint proteins and help activate an immune response against cancer cells. Checkpoint inhibitors work by blocking signals that cancer cells use to hide from the immune system. In breast cancer, these drugs target the PD-1 or PD-L1 signal receptors—proteins that are either on a tumor’s immune cells or cancer cells.
TNBC and immunotherapy
One impediment to using other breast cancer treatments on triple-negative breast cancer (TNBC) is that these tumors don’t have any of the receptors commonly found in breast cancer—those for the female hormones estrogen and progesterone, and for the human epidermal growth factor (HER2) protein. The U.S. Centers for Disease Control and Prevention compares these receptors to locks on a house that doctors can open with keys—or treatments—to get inside to attack the cancer. TNBC doesn’t have any of the three locks, which up until recently meant few treatment options other than chemotherapy.
But triple-negative breast cancer also tends to have higher levels of tumor-infiltrating lymphocytes, which may be activated by a checkpoint inhibitor. Research shows that patients with triple-negative breast cancer, which accounts for up to 20 percent of all breast cancers, appear to respond better to checkpoint inhibitors than patients with other types of breast cancer.
Breast cancer immunotherapies
The two FDA-approved breast cancer immunotherapies are:
- Atezolizumab (Tecentriq®), approved for use in March 2019. This drug tries to boost the body’s immune response by blocking PD-L1, thereby shrinking the breast cancer cells or slowing their growth. Atezolizumab is authorized for use with the chemotherapy drug Abraxane® (albumin-bound paclitaxel) to treat advanced triple-negative breast cancer tumors that express the PD-L1 protein. The drug combination may also be used as an initial treatment for some patients.
- Pembrolizumab (Keytruda®), approved for use in November 2020. This drug tries to boost the body’s immune response by blocking PD-1 and shrinking tumors. Pembrolizumab is used in combination with chemotherapy when treating TNBC that recurs locally and can’t be removed by surgery, or when the cancer has spread to other parts of the body. The treatment is only for tumors that have not previously been treated with chemotherapy.
Pembrolizumab was previously approved by the FDA in May 2017 for use based on a cancer’s genetic features found in its DNA. The approval applied to tumors with specific genetic features: microsatellite instability-high (MSI-H), mismatch repair deficiency (dMMR) or high tumor mutational burden (TMB-H). It was the first FDA approval of a cancer drug that wasn’t based on a tumor’s primary location. The gene mutations targeted by pembrolizumab are more commonly found in gastric cancers, but are sometimes found in breast and other cancers.
The overall effectiveness of atezolizumab in treating triple-negative breast cancer is still being evaluated, and trials have not always been as successful as researchers had hoped. For instance, a recent clinical trial found that when the drug is used with a version of the drug paclitaxel other than Abraxane, atezolizumab “failed to improve either progression-free survival or overall survival in advanced triple-negative breast cancer patients, irrespective of PD-L1 status,” according to a recent article in Cancer Today, a publication of the American Association for Cancer Research. In September, the FDA issued an advisory against the use of atezolizumab with paclitaxel.
Immunotherapy studies continue
Researchers continue to look for new ways to use immunotherapy to treat breast cancer. Early research released in November from a Purdue University study shows promise in focusing on reprogramming immune cells that are acting as tumor accomplices, rather than producing checkpoint inhibitors that activate the immune system to attack the cancer.
The Purdue study used a toxin that, when attached to the immune cells, may kill cancer cells. Instead of creating a lab-produced antibody to target the problem immune cells, the study linked folate, a form of vitamin B, to the toxin. Researchers said two factors may promote the success of this approach:
- The affected immune cells love folate and have receptors for it, unlike most other cells in the body, which helps the toxin target the tumor region.
- The folate goes through the body quickly and then is passed out in urine, which is important in removing the lethal toxin attached to any remaining folate from the body.
"We use the vitamin folate to target attached drugs specifically to these nonmalignant cells within a tumor mass that, unfortunately, promote tumor growth. These tumor-associated macrophages [TAMs] love folate," Philip Low, Purdue's Presidential Scholar for Drug Discovery and a chemistry professor, said in a university news release. "They have an enormous appetite for it. They take it up right away, and if they don't, the compound passes in the urine within about 30 minutes. So, we're using folate as a kind of Trojan horse to trick the tumor-promoting immune cells into eating a drug that will reprogram them into tumor-fighting immune cells."
These non-malignant cells in the tumor are called TAMs or myeloid-derived suppressor cells (MDSCs), which are a major force behind suppressed immune responses in many cancer types. When these immune cells infiltrate a solid tumor mass, the cancer cells retrain them so that they allow the tumor to keep growing, Low said. A May 2019 National Institute of Health report described MDSC cells as a promising target for cancer research.
Clinical trials for immunotherapy drugs
While few immunotherapies have been approved for breast cancer to date, studies of other potential immunotherapy treatments are underway. Some breast cancer patients who aren’t eligible for the currently available immunotherapies may qualify for clinical trials researching others.
Trials may allow doctors to prescribe drugs as off-label treatments, testing the drugs for their effectiveness in treating cancer types for which they have not received FDA approval. Patients participating in the Targeted Agent and Profiling Utilization Registry (TAPUR) study, for instance, may be prescribed anti-cancer drugs by matching them to specific genomic mutations found in their individual tumors.
“There are a number of immunotherapy trials, including trials for early-stage breast cancer, at CTCA,” Dr. Farrington says. Those trials include potential treatments for hormone receptor-positive (ER+) and HER2+ breast cancers, she says.
Learn how doctors, researchers re-thinking metastatic cancer treatments.