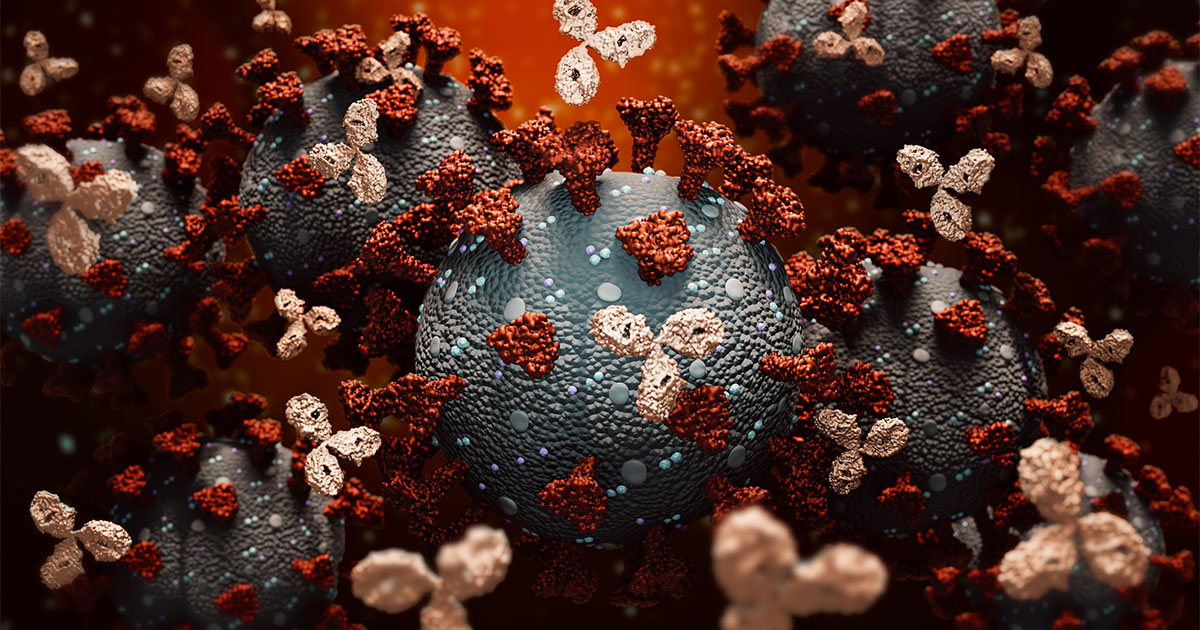
While vaccines may eventually reduce the number of COVID-19 infections, therapies are needed to treat those who still get sick from the virus. Some scientists developing new treatments for those with COVID-19 symptoms are turning to the same biomedicine playing an increasingly important role in treating cancer: monoclonal antibodies. These re-engineered immune proteins are part of a rapidly developing field known as precision medicine. For cancer patients, they’re used in targeted therapy and immunotherapy drugs.
What are monoclonal antibodies?
In immunotherapy, monoclonal antibodies may be used to block signals that cancer cells send to evade the immune system. Monoclonal antibodies are much more commonly used in targeted cancer therapy, where they’re designed to attach to antigens found on cancer cells. Monoclonal antibodies used in targeted therapy include:
- Naked monoclonal antibodies, engineered to stop cancer cell growth or cause the cancer cells to self-destruct
- Conjugated monoclonal antibodies, designed to carry chemotherapeutic agents or radioactive substances to tumor cells to cause cell death
- Bispecific monoclonal antibodies, two monoclonal antibodies that can attach to two different proteins at the same time
Monoclonal antibody treatments have been around for 35 years. The U.S. Food and Drug Administration (FDA) has approved about 100 monoclonal antibodies for therapies, with about a third of those treating different types of cancer. Another 570 are being studied, with roughly 70 percent of those designed as cancer treatments.
Ankur R. Parikh, DO, Medical Director of Precision Medicine at Cancer Treatment Centers of America® (CTCA), says each type of monoclonal antibody is narrowly designed to attach to a specific antigen on a cell. “It’s a specific molecule that we’re using that targets the actual cancer itself and so, therefore, gives patients potentially better responses than just standard chemotherapy, which kills anything, good and bad,” Dr. Parikh says.
These drugs may cause fewer side effects “because you’re not necessarily targeting other parts of your body that you don’t need to be,” and the treatments may produce better results because they’re “really focusing on the problem at play,” he says.
The irony in the promising potential of treating cancer with monoclonal antibodies is that the process uses a cancer cell—an immortal myeloma cell line—to replicate the millions of antibodies needed for each therapy. The same trait that causes cancer to grow unchecked inside the body is repurposed in the laboratory to manufacture countless armies to battle cancer or other diseases.
Monoclonal antibodies and COVID-19
The FDA has given emergency use authorization for several monoclonal antibodies to treat high-risk COVID-19 patients. However, these treatments still may not be widely used, and their supply has significantly exceeded the demand. There may be several reasons for the reluctance to use this form of therapy:
- Many hospitals have been overwhelmed with COVID-19 patients and don’t have the resources needed—additional staff, segregated space and time—to provide the infusions.
- No randomized clinical trials—the “gold standard” of research—have been conducted showing proof that the monoclonal antibodies actually work.
- Patients may not be aware of the availability of this treatment. Federal health officials are encouraging high-risk COVID-19 patients to question their health care providers if they aren’t being offered it.
- Infusions are thought to be effective only within the first week of COVID-19 illness.
Unlike some COVID-19 treatment guidelines, monoclonal antibody therapies for cancer aren’t time-sensitive. This may be related to the nature of the illnesses, says Jeffrey Hoag, MD, Chair of the CTCA® Department of Medicine.
The goal of the COVID-19 treatment is to quickly lower a patient’s overall viral burden, Dr. Hoag says. The hope is to reduce the possibility of an inflammatory response that causes severe illness and potentially leads to hospitalization, ventilation or death. Monoclonal antibody therapies for cancer, on the other hand, usually aren’t targeting an inflammatory response; they try to stop cancer cells from replicating or kill them off gradually.
“Repeat dosing is the norm for these treatments because the goal is to persistently suppress the cancer from growing, or kill the cancer cells over time,” Dr. Hoag says. He compares infusing monoclonal antibodies into a COVID-19 patient to dousing a fire with water, reducing the flames to embers. But cancer is more like a forest fire, where a monoclonal antibody treatment acts as a controlled burn around the cancer, denying it the fuel it needs to spread and trying to choke it out over time through multiple treatments.
A COVID-19 prevention?
In January, a clinical trial suggested that some monoclonal antibody treatments may prevent COVID-19 infection. The research, conducted by the National Institute of Allergy and Infectious Diseases, found that an Eli Lilly antibody treatment, bamlanivimab, significantly reduced the risk of contracting COVID-19 symptoms in residents and staff at long-term care facilities.
Researchers say such immunity may last for only a short period of time, but it may be useful in residential housing complexes experiencing a COVID-19 outbreak and an inability to get vaccine to residents in a timely manner. The results showed people receiving the monoclonal antibody therapy had an 80 percent reduced risk of catching the virus than untreated nursing home residents.
While not approved as a potential COVID-19 vaccine, the drug has been approved by the FDA to treat mild to moderate COVID-19 in some high-risk patients.
Understanding antibodies
The body has several layers of defense against viruses, bacteria and other invaders. Germs that get past the skin or mucous membranes are met by the cells of innate immune system, such as dendritic cells and macrophages, that attack the invaders and alert T-cells and B-cells of their presence. T-cells kill the invading cells and retain information about their antigens to recognize them should they attack again, while B-cells produce antibodies tailored for antigens found on specific cells.
Sometimes, as with cancer, the body’s immune system doesn’t recognize an invader. Or, as with COVID-19, it’s a new disease that humans haven’t faced before and the immune system has trouble attacking. That’s why scientists have turned to the laboratory to engineer man-made antibodies to succeed where natural defenses have failed.
Types of monoclonal antibodies
Monoclonal antibodies are made in four different ways, with each type given a different suffix depending on the process used, such as:
| Type | Source | Suffix |
|---|---|---|
| Murine | Mouse proteins | omab |
| Chimeric | a combination of mouse and human proteins | ximab |
| Humanized | Small parts of mouse proteins attached to human proteins | zumab |
| Human | Human proteins | Umab |
Drugs ending in the suffix “vimab,” such as the COVID-19 drug bamlanivimab, have antiviral properties.
How monoclonal antibodies are made
To make monoclonal antibodies, scientists look for an appropriate antigen on a cancer cell or other invading cell and try to develop a drug that prompts B-cells to connect to that specific antigen. The drug is then injected into an animal or human—depending on the type of monoclonal antibody being produced—to create B-cells that produce the antibodies programmed to work against that specific antigen.
Scientists filter the resulting B-cells in the lab to determine which of the new antibodies binds best with the targeted antigen. The selected antibody is then fused with a myeloma cell, creating a hybridoma—a monoclone—that continuously reproduces the same antibody for future therapies.
Side effects from monoclonal antibodies
Monoclonal antibodies are usually given by injection or infusion. Patients whose treatment plans include more frequent injections or infusions may choose a port or catheter to deliver their drugs more efficiently and with less pain.
Potential side effects include:
- Fever
- Chills
- Weakness or fatigue
- Headache
- Nausea or vomiting
- Diarrhea
- Low blood pressure
- Rashes
These side effects often are less severe than those experienced by some patients on systemic treatments, such as traditional chemotherapy, Dr. Parikh says. “The main thing you see is allergic reaction, because you’re using sort of an immune system response similar to certain immunotherapies,” he says. “So, most people on monoclonal antibodies will not get nausea, or hair loss, or neuropathy, or have lower blood counts—things you think about with chemotherapy.”
The severity of side effects may also depend on the antigen being targeted. Bevacizumab (Avastin®) lowers a tumor’s blood vessel growth and may produce blood-related side effects, such as high blood pressure, poor wound healing or blood clotting. Cetuximab (Erbitux®) targets proteins on skin cells, which may lead to severe rashes for some people.
The future of monoclonal antibodies in cancer treatment
While monoclonal antibodies appear to be a major part of future cancer research, their usefulness is very specific to an individual’s cancer profile. Before determining whether a monoclonal antibody is an appropriate treatment, an oncologist may order tests to help determine which protein may be driving the behavior of the patient’s cancer cells. These tests may include advanced genomic testing, genetic testing or an examination by a pathologist.
Researchers are also trying to determine whether mutations targeted for treatment in one cancer may be found in other cancers, potentially expanding the use of a particular monoclonal antibody therapy.
“We’re doing more molecular profiling on these tumors, identifying more mutations,” Dr. Parikh says. “We’re starting to identify more of these monoclonals and trying to become more targeted in our approach to cancers, realizing that we cannot talk about one size fits all. Everyone’s biology is different; tumors are different.”
Learn how mRNA vaccines for COVID-19 may lead to cancer treatments.