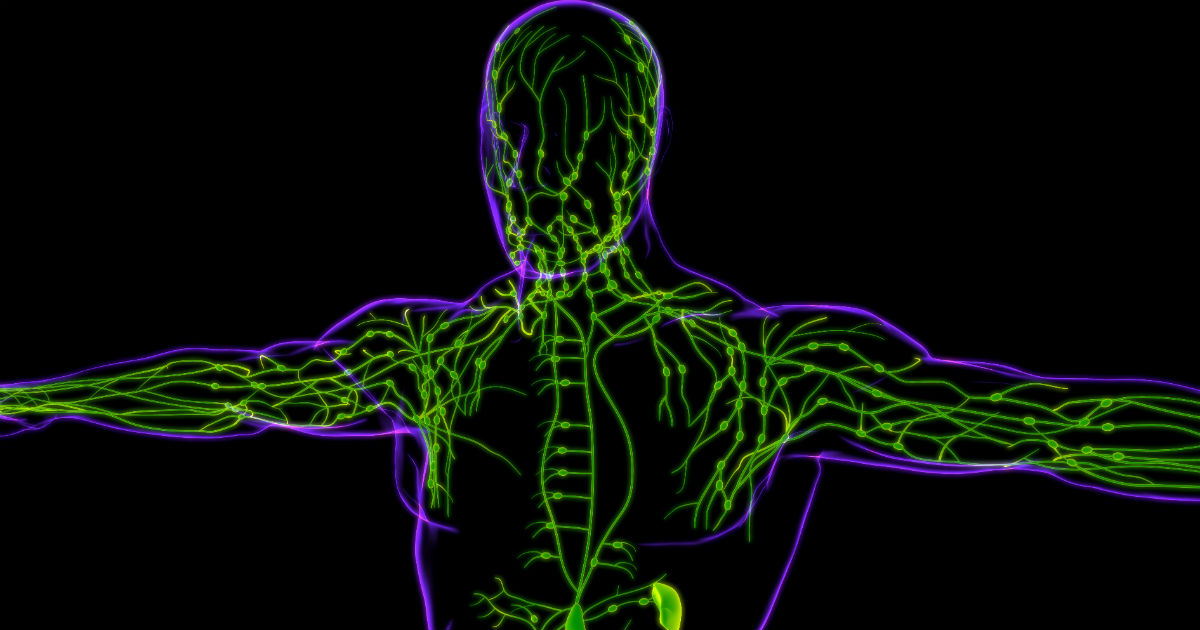
The human body is a collection of networks—systems of parts that work together to keep us alive and well. The bloodstream, for instance, is a network of arteries, veins that carry blood to and from the heart. The central nervous system is a network that reacts to signals sent to and from the brain. A key part of the immune system is the lymphatic network that carries lymphatic fluid to and from our tissue and organs. This fluid contains lymphocytes—white blood cells responsible for fighting infection and disease. The lymphatic system also filters out harmful substances, such as bacteria, from lymph fluid before returning it to the bloodstream.
Cancer and its treatments, especially surgery and radiation therapy, may sometimes change, block or interrupt the flow of lymph fluid through the lymphatic system. When this edema develops from a build-up of lymphatic fluid, it’s called lymphedema. This abnormal collection of fluid causes swelling in specific areas of the body, most often in the arms or legs.
If untreated, lymphedema may lead to decreased function and mobility in the affected limb, skin issues, pain and discomfort and other complications. An accumulation of protein-rich lymph fluid may lead to increased swelling, hardening of the tissue and infection. But with proper care and treatment, lymphedema may be prevented or controlled. And, while lymphedema may cause distress, knowing you have choices in how to manage the condition may help you better cope with the situation while reducing its impact.
Lymphedema and cancer
There are two types of lymphedema:
Primary lymphedema is a rare, inherited condition caused by the absence of, or abnormalities in, certain lymph vessels and nodes. This condition may be present at birth or develop at puberty or in adulthood.
Secondary lymphedema, also called acquired lymphedema, may develop as a result of cancer, cancer treatment, infection, trauma, scar tissue, or anything that changes, blocks, or interrupts the flow of lymph through the lymphatic system.
Lymphedema is most often associated as a side effect of breast cancer. Breast cancer patients are particularly at risk of lymphedema because axillary lymph nodes in the armpit near the breast may be removed or damaged by breast cancer surgery, radiation therapy or a combination of cancer treatments. But lymphedema may also result from treatment for prostate cancer, gynecological cancers, lymphoma, melanoma or other cancers. The more lymph nodes removed or damaged, the higher the risk for developing lymphedema.
Some potential causes of cancer-related lymphedema are:
- A tumor, especially one that blocks the lymph system
- Surgery and/or radiation therapy involving the lymph node region
- Recurrence or spread of a tumor to the lymph nodes
- Infection of and/or injury to the lymphatic vessels
- Inflammation or scar tissue
- Temporary loss of lymphatic function
- Blockage of a vein by a blood clot
Difficult to predict
While we know a lot about lymphedema, predicting who will develop the condition is often difficult. “There is that innate variability among humans,” says Fernando U. Garcia, MD, a Pathologist at Cancer Treatment Centers of America® (CTCA), Philadelphia. “The exact same operation on one patient may not result in lymphedema, while it may on another patient. It has to do with the amount of lymph nodes that you are born with and those left intact—or removed—after surgery. The more lymph nodes the surgeons are able to leave, the less likely you are to develop lymphedema.”
Complicating matters further is that there is no precise timetable as to when lymphedema might occur. The course of lymphedema varies from person to person, and swelling may range from mild to severe. Lymphedema may occur within a few days, weeks, months or even years after surgery or it may occur during or after radiation treatment. It commonly develops slowly, becoming noticeable 18 to 24 months after cancer treatment. Early diagnosis and treatment for lymphedema is important to help reduce symptoms and prevent the condition from progressing.
While lymphedema may develop in any part of the body, it most often affects the arms or legs. For instance, if lymphedema develops after breast cancer treatment, it may affect the soft tissue around the breast and underarm, as well as the arm closest to the surgery site.
Symptoms of lymphedema include:
- Swelling in the arms, hands, fingers, shoulders, chest, or legs
- Indentations of the skin that remain when pressed(an early symptom)
- A weakness or heavy feeling in the arms or legs
- A feeling of tightness or stiffness in the skin
- Pain, heat and/or redness in the affected area
- Aching in the neck, shoulders, spine or hips
- Decreased movement or flexibility in the hand, wrist or ankle
- Difficulty fitting into clothing; tight-fitting ring, watch or shoes
Management and treatment of lymphedema
Lymphedema treatment options vary from person to person, depending on the severity and cause. Treatment may include skin care, manual lymph drainage, gentle massage therapy and light exercises to help stimulate the lymphatic system. Wearing compression bandages, pumps or garments (e.g., sleeves, stockings) may also help prevent additional fluid from accumulating in the tissue. In addition, medications may help reduce inflammation, prevent blood clots and treat infections.
Here are some tips to help cope with lymphedema:
Communicate with your health care team. Better recovery occurs when lymphedema is discovered early, so it’s important to tell your doctor if you experience symptoms. Try to monitor your activities to determine if a particular activity causes the condition to worsen. Also, follow up regularly with your health care team to see that compression garments are well-fitted.
Stay alert for signs of infection. Poor drainage of the lymphatic system may make the affected limb more susceptible to a skin infection called cellulitis. Try to check all areas of the arms and legs daily for signs of infection, which may include redness, pain, tenderness, heat, swelling, and/or rash, as well as a fever over 100° F and chills. Immediately report warning signs of infection to your doctor.
Wear well-fitting compression garments. Compression garments may help prevent swelling by squeezing the lymph fluid through the remaining vessels before it builds up. Compression stockings, sleeves or bandages must be carefully fitted and monitored to apply the right pressure while avoiding too much tightness near the top. Compression garments may help to support the affected limb with a compression garment during strenuous activities or air travel, as long as you do not have open wounds or poor circulation.
Protect the affected area. Try to protect the affected area from scratches, sores, burns, insect bites or other irritations or injuries. Your body may respond by making extra fluid. Keep the skin clean and dry to reduce the risk of infection. Wear protective gloves while doing housework or gardening. Avoid exposure to extreme cold or prolonged heat, which may be associated with increased fluid build-up, swelling or chapping/chafing of skin.
Limit certain activities. Avoid muscle strain, vigorous activities, repetitive movements, heavy lifting or pulling of the affected limb. Also, avoid prolonged lying, standing, sitting or crossing the legs on the affected side. These activities may increase the pressure in nearby blood vessels, which may lead to increased swelling. If possible, try to avoid having blood pressure taken, blood drawn or injections given on the affected side as well.
Maintain proper nutrition. Eating a well-balanced diet may help the body tolerate cancer treatments, fight infection and rebuild tissue. Try to maintain a healthy weight, since obesity may increase the chances of swelling. Avoid foods high in salt and fat. A registered dietitian may help develop an appropriate meal plan for you.
Stay active. Exercise and activity may help stimulate the lymphatic system and improve lymphedema by helping to drain lymph fluid from the limbs. However, it is important to gradually increase the intensity of activity and avoid fatiguing the muscles of the affected area, which may cause injury or additional fluid accumulation. A rehabilitation therapist may help develop an individualized exercise program for you.
Dress comfortably. Wear comfortable, well-fitting clothing and shoes. Women should wear well-fitted bras, and bra straps should not be too tight. Avoid socks, hosiery or undergarments with tight elastic bands. Wear loose watches, jewelry, and gloves. Avoid carrying handbags on the affected arm.
Get pain under control. You may experience pain caused by the swelling and pressure on nerves, loss of muscle tissue and function, or scar tissue. Your doctor may treat your pain with medications, relaxation techniques or other methods.
Consult with a rehabilitation therapist. Your doctor may refer you to a rehabilitation therapist trained in managing lymphedema. A rehabilitation therapist may assess your condition and work with you to develop an individualized lymphedema management plan.
Seek emotional support. In addition to physical challenges, lymphedema may cause emotional difficulties. If you need additional assistance to cope with lymphedema, talk with your doctor about counseling and other available resources. Support groups may be a great source of emotional support.


