At a time when more people are surviving cancer than ever before, the incidence rate of primary liver cancer is seeing a meteoric rise. A December 2018 JAMA Oncology study found that liver cancer diagnoses increased by 75 percent worldwide between 1990 and 2015. In the United States, the number of diagnoses has more than tripled since 1980, and liver cancer is now the fastest-growing cause of cancer death. To explain the jump, many experts point to the simultaneous upswing among the leading causes of the disease: alcohol use, hepatitis infection and obesity. But many of these risk factors are preventable. And, for those that aren’t, research in recent years has led to new treatment options, and an increased focus on screening and prevention.
“I think we’ve seen a boom lately in liver cancer treatments. Even as few as five years ago, liver cancer seemed to be an ugly duckling. No one wanted to dedicate their career to treating the cancer type. Now, with the advent of immunotherapy and targeted treatments, the interest in liver cancer is growing.” – Arturo Loaiza-Bonilla, MD, MSEd, FACP, Vice Chair of the Department of Medical Oncology at Cancer Treatment Centers of America® (CTCA)
The liver has many important functions, including secreting bile for digestion and synthesizing proteins. It also breaks down everything we eat and drink, including alcohol, and filters toxins from the blood, says Pragatheeshwar Thirunavukarasu, MD, Surgical Oncologist and Hepatopancreaticobiliary Surgeon at our hospital in Tulsa. If we consume too many harmful substances, though, the liver is forced to work harder. “Whenever there is an insult to the liver, whether from alcohol, drugs, hepatitis or fatty deposition, cells begin to die,” Dr. Thirunavukarasu says. Although the liver can regenerate itself, if the same damage continues for several years or decades, the organ may become permanently scarred, a condition called cirrhosis. Early symptoms of cirrhosis include jaundice and a swollen abdomen, but once it advances, it may cause severe internal bleeding, kidney failure, brain injury and liver cancer.
Incidence of risk factors on the rise
Cirrhosis can occur for a number of reasons, but it has a few common culprits. One is alcoholic fatty liver disease, or AFLD, which occurs when heavy alcohol use causes liver scarring. According to the American Institute for Cancer Research, liver cancer deaths are “largely caused by consuming high amounts of alcohol.” That research is consistent with reports that have found more and more Americans are drinking alcohol, and abusing it. From 2002 to 2013, in fact, drinking among U.S. adults increased by 11 percent.
Another common cause of cirrhosis is infection with the hepatitis B or hepatitis C virus, which targets the liver and typically leads to inflammation. Hepatitis may be spread through sexual intercourse, childbirth, tattoos or piercings with unsterilized equipment, and the sharing of needles or personal items, such as a toothbrush. Because hepatitis infections cause few symptoms, many people who have the disease—more than half, according to the U.S. Department of Health & Human Services—don’t know they have it.
In 2017, the U.S. Centers for Disease Control and Prevention (CDC) found that new cases of hepatitis C infection tripled between 2010 and 2015. According to the report, three-quarters of the 3.5 million Americans living with hepatitis C are baby boomers born between 1945 and 1965, which was before screening for the virus became common practice. But the study also found that those with the highest overall number of new infections were aged 20 to 29—a trend the CDC attributes, in large part, to the opioid epidemic.
When it comes to hepatitis B, the incidence of new cases had been on the decline before the early 2010s. But in 2013, nearly 20,000 acute cases of the infection were reported, representing an increase of more than 5 percent compared to 2012, and the first time in more than 20 years that the number of acute infections increased.
A third common cause of cirrhosis is non-alcoholic fatty liver disease, or NAFLD, which is often associated with a poor diet, sedentary lifestyle and obesity, the latter of which hit an all-time high in the United States in 2016, with 39.8 percent of the adult population categorized as obese. The trend was further documented in a 2017 study published in Nature Genetics that found 30 percent to 40 percent of U.S. adults had NAFLD, which may raise the risk of heart disease, diabetes, cirrhosis and liver disease. And cases of NAFLD are forecast to increase by 21 percent, from 83.1 million in 2015 to 100.9 million in 2030.
Because many of the factors that contribute to liver cancer are lifestyle-related, the risk of developing the disease may be reduced with certain behavioral changes, like losing weight, limiting alcohol use, sticking to a healthy diet and refraining from the use of injectable drugs. In fact, a study published in late 2018 in CA: A Cancer Journal for Clinicians found that about 71 percent of liver cancer diagnoses in the United States are attributable to preventable risk factors, such as obesity and excessive alcohol consumption. On the positive side, tobacco use, which the study says causes 22 percent of liver cancer deaths, is on the decline.
Prevention and treatment
For risk factors that aren’t linked to behavior, such as some hepatitis cases, research over the past decade has led to certain prevention initiatives designed to help. For instance, people who are at risk for hepatitis B may receive a vaccine to help prevent the disease, and new antiviral medications may help treat hepatitis C.
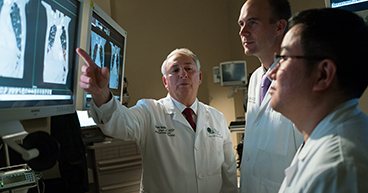
“Many liver cancer cases can be prevented, but we, as doctors, can’t do much, if anything, about obesity, smoking, alcohol or other lifestyle-directed factors right now,” Dr. Bonilla says. “We can do something, however, about risk factors we can control, like hepatitis B and C. More people are getting vaccinated against hepatitis B today and there’s a much greater awareness of the importance of getting screened for hepatitis C. I think with the increased interest in the treatment of hepatitis C, we’re going to have more patients followed closely because we now have treatment options for those patients.” Typically, primary care doctors routinely test for liver damage and, if damage is found, screen every six months to a year for nodules that may suggest cancer.
Once liver cancer develops, however, it is typically difficult to treat, Dr. Bonilla says. “The first reason is because it’s usually not detected until it’s advanced and difficult, if not impossible, to remove surgically. The second is because cancer cells often invade blood vessels in the liver, which may not be surgically removed, and the third is because patients may not be able to handle more aggressive treatments because the liver is already damaged by whatever factors led to the cirrhosis, such as hepatitis or chronic alcohol use.”
In fact, only a limited number of liver cancer patients are eligible for surgery, Dr. Thirunavukarasu says. Those patients must have tumors that are small enough to be removed, and they must be otherwise healthy enough to undergo surgery. For example, a patient with a high Child-Pugh score, a test that measures a patient’s underlying liver function, may not be deemed stable enough to receive some treatments. “Liver transplants are the preferable option for treating early liver cancer, but it’s only an option for a minority of patients,” Dr. Thirunavukarasu says. “Usually, the limiting factor is not the treatment; it’s the patient’s ability to get the treatment.”
Liver failure is a significant complication, he added. “It cannot be treated; it can only be optimized,” Dr. Thirunavukarasu says. “The same is true with cirrhosis.” When a person has cirrhosis, another disorder called portal hypertension often follows, developing when scar tissue in the liver blocks the flow of blood through the organ and slows its ability to function. Cirrhosis may also cause hepatic encephalopathy, a loss of brain functioning when the damaged liver can no longer remove toxins from the blood. “Both portal hypertension and encephalopathy are caused by advanced liver disease,” Dr. Thirunavukarasu says. “Often times, patients come in with symptoms of one of these conditions, and it’s only then that we find they also have liver cancer. We cannot operate on these patients. We can do things to help, but the only way to treat severe liver damage is with a liver transplant, and the vast majority of patients aren’t eligible for a transplant.”
Over the past few years, the targeted therapy drugs sorafenib (Nexavar®), regorafenib (Stivarga®), lenvatinib (Lenvima®) and cabozantinib (Cabometyx®), and the immunotherapy drugs nivolumab (Opdivo®) and pembrolizumab (Keytruda®), have been approved to treat certain cases of liver cancer that aren’t able to be treated with surgery or a transplant. At CTCA®, clinical trials combining some of these therapies are available for patients who qualify.
Interventional radiology techniques also may be used when a liver cancer patient doesn’t qualify for surgery or a transplant. These techniques may include hepatic chemoembolization, which blocks the flow of blood to the tumor and delivers a high dose of chemotherapy or radiation directly to the cancer, or hepatic radiofrequency ablation, which uses heat to burn the tumor away.
“Treating liver cancer is an area that hasn’t seen a lot of improvement until recently,” says Issam Alawin, MD, Medical Oncologist at our hospital in Tulsa. “In the past few years, though, we finally have new drugs and treatment options approved to help with this disease.”
Learn more about less aggressive treatment approaches now available for certain cancers.