Lung cancer has long held the notorious distinction as the deadliest cancer in America. The disease kills nearly 160,000 U.S. men and women each year and accounts for one in four cancer deaths, claiming more lives than colon cancer, breast cancer and prostate cancer combined. But many experts believe they’re witnessing a turning point in the fight against lung cancer, for two reasons: More novel drugs are being approved to treat advanced cases, and oncologists now know more than ever about the disease they’re battling. “The future of lung cancer treatment looks very bright,” says Ashish Sangal, MD, Medical Director of the CTCA® Lung Cancer Center, Phoenix and Medical Oncologist at our Phoenix hospital. That optimism stems, in large part, from a shift in treatment paradigms—from a one-size-fits-all approach to more individualized care.
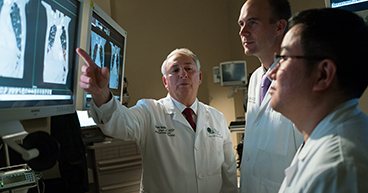
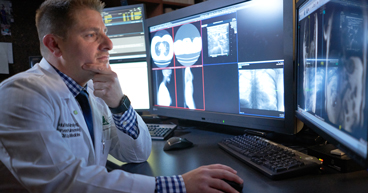
Oncologists lump lung cancer into two categories: non-small cell, which makes up nine out of 10 lung cancers, and small cell, which represents less than 20 percent of lung cancers. A decade ago, treatment decisions required little additional information. Each type was treated with basically the same techniques, typically surgery for early-stage lung cancers and chemotherapy for those in the advanced stages. Today, lung cancer treatments are determined by far more than the type and stage of the disease. If the cancer is non-small cell, for example, oncologists determine whether it is squamous cell or adenocarcinoma, the two main subtypes of non-small cell lung cancer. They also perform genomic testing on some patients to look for mutations that may be driving the tumor’s behavior. “Once we know all of these things, we can determine how to treat the cancer,” says Patricia Rich, MD, Medical Oncology Director of the CTCA Lung Cancer Institute and Medical Oncologist at our Atlanta hospital.
Treatments for early-stage non-small cell lung cancer have changed little over the years—the go-to first-line treatment is still surgery, with radiation and chemotherapy among the common alternatives. But more recently, oncologists and drug developers have begun expanding treatment options for patients whose cancer has spread to other areas of the body. The vast majority of these efforts have targeted non-small cell lung cancer, which accounts for 85 percent of cancer in the lungs.
New drug approvals
Over the past few years, the U.S. Food and Drug Administration (FDA) has approved new drugs developed to target specific genomic changes that help non-small cell lung cancer cells grow. Some of these targeted therapies work by stopping the cancer cells from forming new blood vessels; others are designed to neutralize DNA mutations in certain protein receptors, such as EGFR, ALK and BRAF, in order to stop the cancer cells from growing and dividing. “It’s a very small subset of people that these targeted drugs can help, unfortunately,” Dr. Sangal says. “Only about 15 percent of non-small cell lung cancer patients have an EGFR mutation, and only about 5 percent have an ALK mutation, for example. But you get such a good response from these patients with these drugs that it’s a no-brainer.”
Oncologists also recognize they have more to learn about how targeted therapies can be used as the patient’s cancer changes and evolves. “Even if a targeted therapy works and a person’s cancer goes away for a year or two, it may come back because the cancer forms a second or even a third mutation,” Dr. Sangal says.
“ It's almost like a punch and a counterpunch. Cancer forms new mutations, and we have to find new drugs to block those new mutations." - Ashish Sangal, MD
The FDA has also recently approved several immunotherapy drugs called checkpoint inhibitors to treat non-small cell lung cancer: pembrolizumab (Keytruda®), nivolumab (Opdivo®) and atezolizumab (Tecentriq®). These drugs target the PD-1 and PD-L1 cell receptors, which help regulate immune response. The therapies are only approved in patients with certain types of non-small cell lung cancer that hasn’t responded to chemotherapy or other treatments. Pembrolizumab is also approved as a first-line treatment in some patients, either in combination with chemotherapy or by itself.
In addition to treating the cancer, immunotherapies also may mean a better quality of life for some patients, because their side effects, such as fatigue and nausea, are typically less severe than those associated with chemotherapy and other conventional treatments. But for a small number of patients, immunotherapy may cause severe, life-threatening reactions. “Sometimes, when you use immunotherapy to turn off the signal, the immune cells will recognize cells as the enemy, when they are actually good cells, and attack them,” says Daniel Nader, DO, FCCP, FACP, Chief of the Division of Pulmonary Services at Cancer Treatment Centers of America® (CTCA). In such cases, the liver or colon may become inflamed, and treatment may have to be delayed or stopped altogether.
Exploring combination therapies
Still, despite the drugs’ limitations, oncologists are optimistic about immunotherapy’s future for lung cancer patients. “I see more trials of checkpoint inhibitor drugs and better selections for patients coming,” Dr. Rich says. “The more we know about checkpoints and how to work with them to treat patients, the more and more drugs we’re going to see out there that can treat more and more mutations.” For instance, a September study published in The New England Journal of Medicine found that patients with stage III non-small cell lung cancer who were treated with chemotherapy and radiation, followed by the checkpoint inhibitor drug durvalumab (IMFINZI™), lived longer than those treated with chemotherapy and radiation alone. “I think that application is going to be approved,” Dr. Rich says. “And that’s probably the next thing—sequential immunotherapy for non-small cell lung cancers that have spread and can’t be surgically removed.”
Other combinations showing promising results are on the horizon, Dr. Sangal says. “Treatments are becoming very individualized to what type of cancer the patient has,” he says. “It’s not about just picking a treatment out of a bag. It’s about determining where the patient belongs in the broad spectrum of factors.”
Learn more about how the immune system works in both feeding and fighting cancer.