Breast cancer is not a single disease, but instead a range of diseases, each with its own genomic characteristics. Each molecular subtype is treated differently than the others and with different outcomes. Some breast cancers may be aggressive and unpredictable; others are less biologically aggressive.
Doctors are increasingly using genomic information about breast cancer cells to categorize these cancers, typically classifying them into at least four major subtypes: Luminal A and Luminal B, triple negative and human epidermal growth factor receptor 2 positive (called HER2 for short). About one out of every five breast cancers are HER2-positive.
What is HER2?
HER2 is a gene found in healthy cells, but when it mutates, the body makes too many HER2 proteins, which may lead to breast cancer. Understanding the chemical and genetic makeup of your cancer, including whether it’s HER-2 positive, may help doctors recommend a specific treatment and predict how likely the tumor will respond. Invasive breast cancers are typically tested for HER2 levels in a hospital laboratory, using a sample of breast cancer tissue removed during a biopsy or breast cancer surgery.
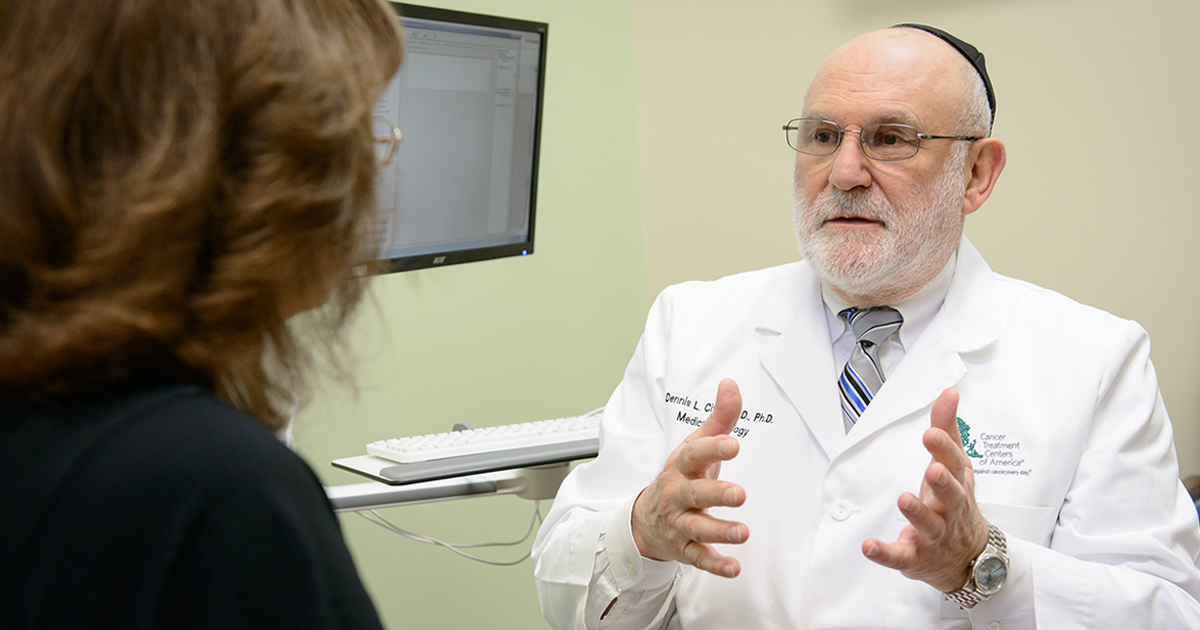
“HER2-positive breast cancers are complicated,” says Dennis Citrin, MB ChB, PhD, Medical Oncologist at our Chicago hospital. “Compared to other breast cancer types, HER2 grows rapidly, is biologically more aggressive and is more likely to metastasize. But we now have drugs designed to target the HER2 protein. The introduction of Herceptin® (trastuzumab) was a watershed moment. I believe the most monumental advancement in the treatment of breast cancer within the past 20 years is the identification of HER2 and development of HER2-targeted treatment. Now we have five approved FDA drugs for HER2-positive breast cancer: trastuzumab, pertuzumab (Perjeta®), lapatinib (Tykerb®), ado-trastuzumab emtansine (Kadcyla®) and neratinib (Nerlynx™).”
Drugs like trastuzumab are called targeted therapies and are designed to stop the growth and spread of cancer cells. Targeted drugs typically have different and often less severe side effects than chemotherapy. “Typically, HER2 drugs are well tolerated and usually do not cause hair loss,” says Dr. Citrin. “But as a precaution, we have to monitor the liver and heart function of patients on targeted therapy drugs.”
Treating HER2-positive breast cancer
Certain standard chemotherapy drugs may also be used to treat HER2-positive breast cancers, although these drugs don't specifically target the HER2 protein. Because some breast cancer patients do not benefit from existing HER2-targeted treatments, and others have become resistant after being on the treatment for a certain period of time, researchers continue to test new or modified drug combinations, including drugs designed to destroy cancer cells without causing side effects.
Research published recently in the New England Journal of Medicine found pertuzumab significantly improved the outcomes of patients with HER2-positive, operable breast cancer when it was used in combination with trastuzumab and chemotherapy. Patients who received both drugs together had a 19 percent lower risk of recurrence of invasive disease compared to those who were treated with trastuzumab alone. Because both bind to the HER2 receptor, though in different locations, pertuzumab and trastuzumab are believed to complement each other.
Several other clinical trials are investigating various treatment combinations for HER2-positive breast cancer. Some studies have also found immunotherapy may be a promising breast cancer treatment option. “Immunotherapy for breast cancer is an active area of research,” says Dr. Citrin. “There may well be a role for immunotherapy in treating some breast cancers.”